What is Achalasia?
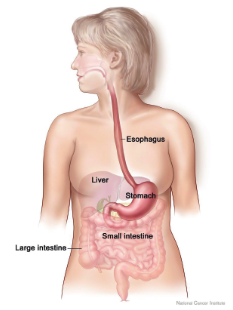
Achalasia is a rare swallowing condition that prevents the food you swallow from reaching your stomach properly. It affects the muscles in your oesophagus, the food pipe that runs from your throat, down through your chest and to your stomach. (In America and some other parts of the world, the spelling is esophagus). In a normal oesophagus, muscles squeeze the food down towards the stomach by tightening and relaxing in a coordinated sequence in a process called peristalsis. At the lower end of the oesophagus, a valve-like ring of muscle (the lower oesophageal sphincter or LOS) should automatically relax to let food through into your stomach. Then the LOS should close again to stop stomach acid from rising. Peristalsis normally takes two or three seconds and is so effective that some people can drink large quantities of liquid whilst upside down.
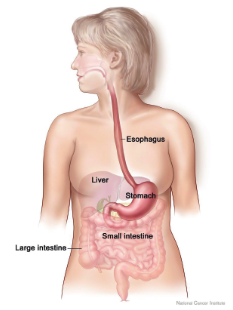
With achalasia, the muscles in the oesophagus do not work properly. They are either weak, do not tighten and relax in the right order, or do not work at all. The LOS, located just above your stomach, often fails to open. Food and drink then block back into your oesophagus and can remain there for a long time, sometimes hours or days. This food build-up can create pressure, similar to a blocked hosepipe, until the food either trickles down into your stomach, or is brought back up through your mouth (regurgitation). This is not caused by a fault in the muscles themselves but seems to be a problem with the nerve endings that send signals to the brain to operate those muscles.
What are the symptoms of achalasia?
If you have achalasia you will not always experience the same symptoms as other people in the same way. People with achalasia can have a whole range of severity of symptoms, or sometimes a much milder version. So interpret the list of symptoms, compare them with your own experience and do not take things out of proportion. This booklet aims to be comprehensive, and whilst some of these problems are listed below, you may well not experience all of them. Although this may be difficult, you should try not to feel more anxious about eating, not least because stress and anxiety do tend to make symptoms worse. It is not inevitable that you will necessarily face the more serious problems. We try to give information about how some symptoms can be alleviated.

Food starting to ‘pool’ at the base of oesophagus
Stuck food
The food that remains blocked in your oesophagus can cause discomfort and sometimes pain in your chest area from the extra pressure. It can also cause anxiety and worry about food not going down into your stomach. Food can pool at the bottom of the oesophagus. Food such as rice and bread can cause a congealing problem. Food with a stringy texture and vegetable or fruit skins can also cause particular problems.
Regurgitating of food and ‘drooling’ of saliva
If food residue cannot go down into your stomach, the pressure on your oesophagus can only be relieved by it moving upwards and being regurgitated. People often try and help blocked food go down by carefully taking a drink of warm or cold water or a fizzy drink. In extreme cases people have sometimes used their fingers to alleviate the problem. Sometimes saliva does not flow properly between the oesophagus and the stomach and can become trapped, leading to excess bubbles and saliva needing to be spat out, or drooling (draining outside your mouth). Regurgitation involves food that does not reach the stomach; reflux is acid and other contents from the stomach itself.
Chest pain from spasms
Spasms seem to be caused by pressure on the nerves and muscles from blocked food, but they can also be caused by reflux and other reasons. Sometimes these pains are misdiagnosed as heartburn. Spasms are not well understood. In an informal survey, people with achalasia most often associated spasm with stress, followed by reactions to certain food. As often occurs with pain, the sensation can sometimes be transferred through the nerve system and be felt in other places like the jaw or back. For some people spasms might be their first, or an early, symptom.
Losing weight
Difficulty in swallowing can easily lead to a reduced intake of food and loss of weight. Sometimes this inability to take in food, and the understandable anxiety that arises from this, can lead to young people being wrongly diagnosed with an eating disorder like bulimia or anorexia, despite the fact people with achalasia genuinely want to eat well.
Malnutrition
Nutrition is absorbed into the body through your digestive system, so the reduced ability of food to reach your stomach will eventually affect nutrition levels. Your GP may prescribe special nutrition drinks such as Fortisip.
Effects from fermenting food, and heartburn
If blocked food in your oesophagus starts to ferment, you may feel a nasty taste in your mouth because of this fermentation of stale food. This can be confused with reflux, where acid comes up from the stomach itself.
If achalasia has not been treated, the sour taste is much less likely to be caused by stomach acid because your LOS valve is likely to be too tight to allow the stomach acid to rise in this way. If you have had a dilatation, myotomy without a fundoplication or a POEM, the LOS will inevitably be more relaxed so the cause of the sour taste is much more likely to be stomach acid.
The oesophagus is a sensitive organ. The lining will tend to be irritated by prolonged exposure to stomach acid, and to a lesser extent by fermenting food, depending on what you have eaten. This is because it is different from the lining of the stomach which is designed to withstand the effect of the strong acid that is part of a healthy digestive system.
Heartburn is a pain in the chest area, normally caused by the effect of reflux of acid from the stomach itself, but it is a feeling that can have a variety of causes. Heartburn is a common complaint, normally treated with over-the-counter indigestion remedies like Gaviscon, Rennies or Tums. If heartburn is persistent for more than three weeks you should consult your doctor. Long term reflux can be a significant health problem.
Medication absorption
Achalasia can result in pills remaining stuck in your oesophagus rather than being dispersed into your system through your stomach. This might cause damage to the sensitive lining of your oesophagus as well as the loss of the intended benefit of the medication. A GP or pharmacist can be asked about whether medication can be prescribed in liquid form to reduce this risk.
Choking and coughing fits
Food residue can sometimes flow upwards and find its way into your lungs, especially when you are lying down. You may find it helpful to raise your head and shoulders with pillows, raising part of the mattress of your bed or even considering a bed with adjustable settings.
Chest infections and other respiratory problems
Food residue that flows up your oesophagus and into your lungs can cause infections and pneumonia.
Fatigue or tiredness
Being unable to swallow food can lead to a lack of strength and energy. It can be helpful to ask for your levels of vitamins and minerals to be tested.
Anxiety and depression
Achalasia is a long-term condition that, for some, can affect your quality of life and destroy the pleasure of eating. Some people find relaxation techniques helpful in reducing anxiety and tension.
A weak and fatigued voice
Reflux around the vocal cords can lead to your voice being affected.
How many people have achalasia?
Achalasia is rare, and statistics are not precise. The number of people diagnosed each year (incidence) is similar in most countries, and is estimated as between 0.7 to 1.6 per 100,000 inhabitants per year. The UK population of 66.8 million would therefore, in theory, generate between 467-1,069 diagnoses annually. The prevalence (number of people continuing to be affected by the condition after diagnosis) is regarded internationally as about 10 in 100,000 and is estimated by the NHS to be around 6,000 in the UK. The latest high-resolution manometry techniques may be contributing to more cases being diagnosed.
How old are those with achalasia?
The condition affects both men and women. It is most common between the ages of 30 and 60 years, but it can develop at any age. Some young children are diagnosed with achalasia, and, rarely, it can be present from birth. A study found only 228 UK children under 16 years diagnosed with achalasia in a 10-year period until 2008 but with a rise in the annual rate within that decade{1}.
What causes achalasia?
The muscles within the oesophagus that perform peristalsis are normally automatically controlled by a complex, interlinked system of nerve cells, or neurons. The cause of achalasia is related to the degeneration and malfunctioning of a specific type of nerve cell called ganglia that send signals to the brain to operate the muscles. The loss of function of these neurons impairs the normal mot