Chronic Kidney Disease (CKD)
Definition: 3 months of reduced glomerular filtration rate (GFR) and or kidney damage (abnormal pathology, blood/urine markers, or imaging)
Etiologies: Most common etiologies include diabetes, HTN, HIV, glomerulonephritis, polycystic kidney disease, drug-induced (analgesics and antibiotics), hyperuricemia, multiple myeloma, progression of AKI (like severe obstruction)
Complications of CKD:
- Anemia – due to decreased production of erythropoietin (+ other factors)
- Hyperkalemia – due to decreased potassium excretion
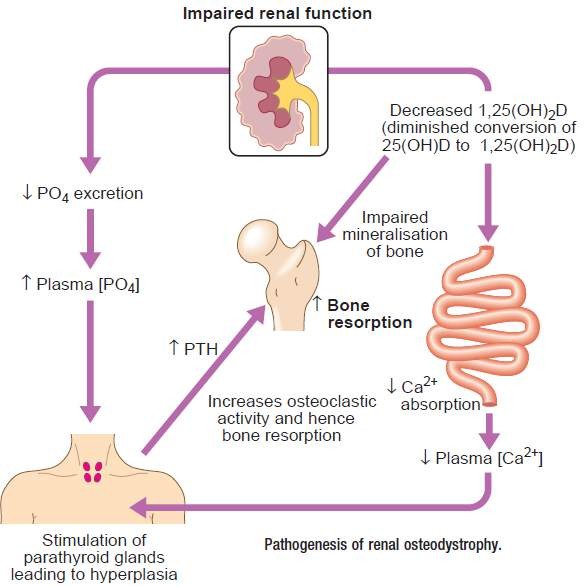
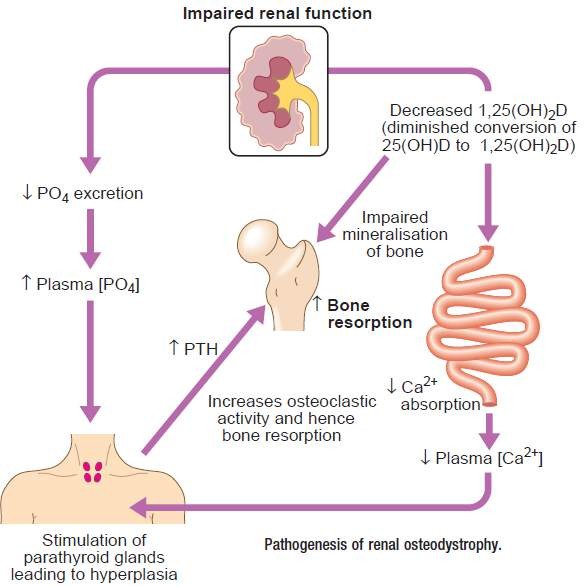
- Hyperphosphatemia / Hypocalcemia – due to decreased phosphate excretion and binding of phosphate to calcium
- Acidemia – due to decreased H+ excretion
- Low Vit D 1,25 / Secondary Hyperparathyroidism / renal osteodystrophy – decreased activation of Vit D causes hyperparathyroidism and painful breakdown of bones
- Edema – due to decreased sodium excretion and hyperaldosteronism
- Uremia - due to decreased excretion of urea and other toxins
|
Signs and Signs of Uremia
|
|
General
|
Nausea, anorexia, malaise, metallic taste, pruritus, uremic frost, muscle wasting
|
|
Neurologic
|
Encephalopathy (change in mental status, decreased memory and attention), seizures, neuropathy, myopathy
|
|
Cardiovascular
|
Pericarditis, HTN, volume overload, CHF, cardiomyopathy, hyperlipidemia, accelerated atherosclerosis
|
|
Hematologic
|
Anemia, bleeding (due to platelet dysfunction)
|
|
Metabolic
|
Hyperkalemia, hyperphosphatemia, acidosis, hypocalcemia, secondary hyperparathyroidism, osteodystrophy
|
Investigations:
- Biochemical: increased urea and creatinine, hyperkalaemia, hypocalcaemia, hyperphosphataemia, and hyponatraemia.
- Urine examination includes microscopy for casts, protein analysis, specific gravity and creatinine clearance.
- Radiology (Pelvi-abdominal US, CTUT)
- Renal biopsy.
Treatment
- Control risk factors for progression of CKD (ex: tight glycemic control if diabetic)
- BP control, goal <130/80, start with an ACEI as first line medication (nephroprotective)
- Monitor for and treat complications: iron +/- erythropoietin to maintain hemoglobin 7-10, low potassium diet / potassium binders, phosphate binders, give Vit D1,25, lasix for edema, dialysis or renal transplant for uremia
- Avoid Nephrotoxins
- A diet low in protein and salt.
- Dose adjustment of drug execrated by kidneys:
Estimating the Glomerular Filtration Rate (GFR) using the Cockroft & Gault equation:
Creatinine Clearance (ml/min) = ( (140-age) x weight (kg) ) / Creatinine (mg/dl) ) X(0.85 in women)
Role of physiotherapy and Benefits of exercise in CKD:
- CKD is associated with malnutrition, secondary sarcopenia, osteoporosis, mobility limitations, and elevated fall risk. Thus, screening for low muscle mass, low bone mass is needed with attention to rapid progression occur with dialysis.
- Renal rehabilitation program should be inclusive to a warm-up and cool down, a strengthening component, a cardiovascular component and flexibility section. The therapist also needs to monitor progression and educate patients in monitoring their progress.
- Dietitian consultation is needed
- Physicians routinely recommend hand squeezing exercises for end-stage renal disease patients with newly placed arteriovenous fistulae (AVF) to increase the rate of fistula maturation.
- Precautions:
- Patients with CKD are mostly hypertensive. So, Blood pressure monitoring pre- session and during is needed.
- Similarly, CKD patients are usually diabetic with same precautions previously mentioned in the section of DM.
- CKD patients fatigue easily with multiple rest break needed.
Hand exercise for AV fistula:
It’s important to exercise the arm both before and after the surgery.
Before surgery: This may make the vein bigger allow fistula to develop.
After surgery: Start doing the exercises 2 weeks after surgery when skin healing occurred
Contraindications for fistula exercises:
- fistula becomes red, hot, painful, swollen, or is leaking (has a discharge)
- the fistula area hurts
- the “thrill” changes or is missing
- the arm or hand on the same side of the body as the fistula gets cold, pale, or blue (suggesting ischemia)
- Resistance Band Wrist Flexion - Patients may consider this exercise to help enlarge their veins in the arm in order to better prepare them for Dialysis days. Using a resistance band, place one end underneath your foot as you sit in a sturdy chair. Hold the other end of the resistance band with your affected arm. Rest your forearm on your thigh with the palm side of your hand facing the ceiling. Bend your wrist up slowly and as far as possible. Your forearm should never leave your thigh. (5 repeatitions)
- Weighted Wrist Flexion - Chronic Kidney Disease patients who are conducting Dialysis should not lift heavy items with their Fistula Arm. Yet, the use of a weight that is three (3) pounds or less may actually be useful in completing a lesser known AV Fistula exercise. If a weight is not available, use a single can of food. Simply, rest your arm on a table so that your wrist is hanging over the edge with your palm down. Grasp the weight in your hand. Slowly raise your wrist and hold it for a few seconds. Lower your wrist again and repeat.
- Resisted Forearm Supination -. Place the palm of the Fistula Arm down on your thigh. Use your other hand to hold the arm in place. Slowly turn your hand up as far as you can while applying light resistance with your opposite hand. Hold this position for a few seconds. Relax and repeat.
- Hand Grips and Stress Balls - These tools are typically used to help the AV Fistula mature, but according to some sources they can also be great exercises to improve the health of an AV Fistula.