Falls
DEFINITION:
Fall is an event whereby an individual unexpectedly comes to rest on the ground or another lower level without known loss of consciousness.
Fall is when a person unintentionally comes to the ground or some lower level not as a consequence of sustaining a violent blow, loss of consciousness, sudden onset of paralysis as in stroke or an epileptic seizure.
EPIEMIOLOGY:
Falls present a substantial health problem among the elderly population. Approximately one third of community dwelling people over 65 years of age will experience one or more fall each year. The frequency increases to nearly 40% for those individuals over 80 years of age. Half of these individuals experience multiple falls and falls affect women more than men.
COMPLICATIONS:
- Falling is an important clinical marker of frailty.
- High mortality rate that is not directly attributable to fall-related injuries.
- Serious injury, such as a fracture, hemarthroses, joint dislocations, sprains, hematomas, severe head trauma, and subdural hematomas.
- minor injuries such as bruises, lacerations, and abrasions.
- Fear of falling, loss of independence and quality of life, One in four fallers report that he or she avoids activities because of fear of falling. As a result of this fear, patients report a poorer quality of life with a loss of function and independence. Impaired mobility because of physical injury.
- Restricted ambulation (either self-imposed or imposed by caregivers).
- An injurious fall sets o a chain of events including emergency department care, hospitalization, surgical intervention, and prolonged immobility. Repeated falls and consequent injuries can be important factors in the decision to institutionalize an older person.
- Falling (injurious or not) has been associated with an increased likelihood of hospitalization, nursing home placement, and death due to older age, chronic conditions, and activities of daily living (ADL) disabilities.
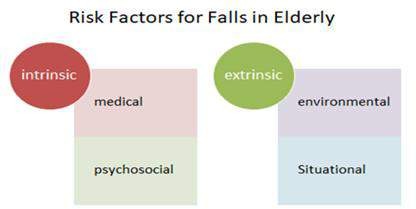
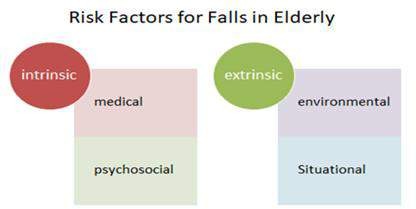
Risk factors:
Intrinsic risk factors include age-related physiologic changes, acute or chronic medical conditions, mobility disorders, balance disorders,and medications.
Age related physiological changes:
- Visual changes that occur with aging include decreased depth perception, decreased dark adaptation, and greater sensitivity to glare.
- Muscular strength in the legs and ankles declines, and joint flexibility also becomes impaired with aging.
- Proprioceptive feedback declines with age, leading to more postural sway.
- The vestibular righting response diminishes with age, thus decreasing the chance of recovering once balance is lost.
- Gait changes that occur with aging include slower speed, decreased stride length, and decreased heel lift.
- Reaction time is prolonged with aging.
- The susceptibility to orthostatic hypotension increases with age.
Medical conditions:
- Acute illness: e.g.pneumonia or myocardial infarction, may present as a fall in an older individual.(Atypical presentation)
- Delirium
- Syncope and Orthostatic hypotension
- Drop attack
- Dizziness
- Dementia (vascular, lewy body) possibly through impairment of judgment, motor function, or visual spatial perception.
- Sensory disorders (vision, hearing, and peripheral neuropathy).
- Foot problem
- Muscle weakness as a result of disuse and deconditioning (caused by pain and/or lack of exercise) can contribute to an unsteady gait and impaired stability
- Healed fractures of the hip and femur can cause an abnormal and less steady gait.
- Residual muscle weakness or sensory deficits from a recent or remote stroke can cause instability.
- Degenerative joint disease (especially of the neck, the lumbosacral spine, and the lower extremities) can cause pain, unstable joints
- Incontinence
- Previous fall
- Fits can cause falls but discussed as separate entity.
Medications:
- Poly-pharmacy itself > 5 drugs.
- Drugs causing orthostatic hypotension: antihypertensive, antianginal, antiparkinsonian, diuretics, antipsychotics, tricyclic antidepressants.
- Sedation, decreased attention: Benzodiazepine, Sedative antihistaminics, ethanol,antiepileptics, antipsychotic, tricyclic antidepressants.
- Extrapyramidal side effects: antipsychotic, metoclopramide.
- Myopathy: steroids, statins, colchicine, interferon, ethanol.
- Miosis of eye: pilocarpine for glucoma
Psychosocial
- Living alone
- Functional dependency
- Depression
- Residential care
- Female gender
- Previous fall
- Low activity, sedentary life
Extrinsic risk factors
Environmental:
- low or elevated bed heights, bed rails, low toilet seats, poorly illuminated areas, upended carpet or rug edges, uneven sidewalks or cur edges, highly polished or wet floors, and icy walkways.
- Unfit walking aid
- Unfit footwear
- Walking bare-feet or only socks
- wear multifocal glasses
- Mechanical restraints
Situational
 During risky activities, such as climbing a ladder or sports activity
During risky activities, such as climbing a ladder or sports activity
 Refuse to use walking aid or glasses
Refuse to use walking aid or glasses
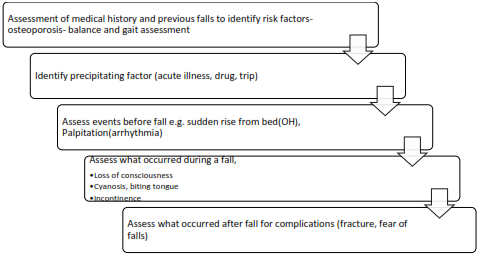
Assessment of Fall:
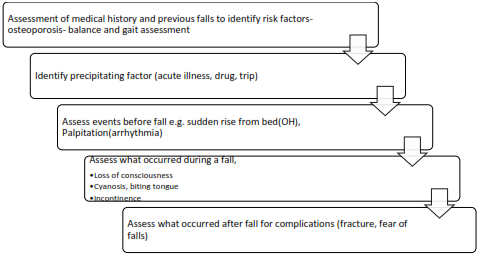
Assessment of medical history and previous falls to identify risk factors- osteoporosis- balance and gait assessment
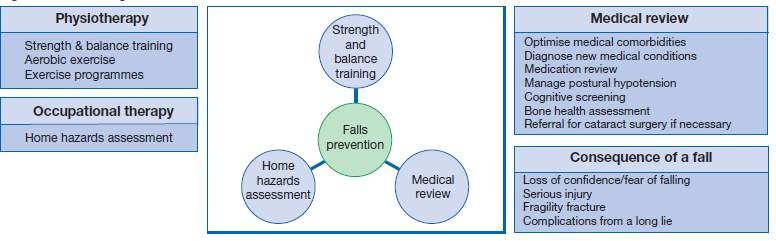
Management:
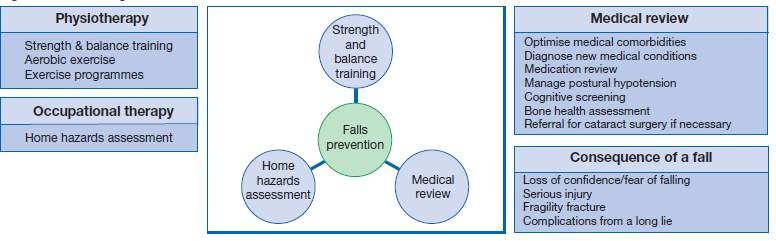
EDUCATIONAL AND HEALTH PROMOTION:
All fall prevention programs include educational and health promotion components. Education of patient and caregiver can be considered as primary and secondary prevention measures and is also important for implementation and sustained use of fall prevention strategies.
RISK FACTOR MODIFICATION:
Home assessment is advisable as part of a multifactorial intervention. It may be covered by Medicare in some cases and should be performed by a trained occupational or physical therapist. There are also a number of home safety checklists that patients may self- administer. The home safety assessment ideally should be tailored to match the specific deficits of the individual.
Important safety issues for hospitals and nursing homes include adequate lighting and handrails in hallways, close monitoring for spilled liquids on the floors, unobstructed walkways, appropriate assistive devices in bathrooms (eg, grab bars, shower chairs, raised toilet seats), furniture that is easy to rise from, and proper bed height.
- CORRECTION OF VISION DEFICITS
Correction of unilateral vision loss should be encouraged to enhance mobility, particularly if the fall is related to tripping or change in depth. Maximal lighting in the home with reduction in glare should be encouraged. Consideration should be given to switching from bifocal to distance lenses, particularly if a fall has occurred on a stair, ramp, or curb. Older adults with poor neck flexion may be more likely to have problems with inaccurate depth perception related to bifocals because they may be unable to flex the neck sufficiently to look at the feet through the upper, distant lenses.
- TREATMENT OF CARDIOVASCULAR ABNORMALITIES
Consideration should be given to further evaluation and treatment for carotid sinus syndrome in the case of otherwise unexplained falls, even in the absence of a history of syncope. Use of a pacemaker in older adults with unexplained falls and cardioinhibitory carotid sinus syndrome has been shown to decrease falls. Treatment of symptomatic orthostatic hypotension should be considered when circumstances of the fall suggest this as a cause. If an asymptomatic finding of orthostasis is noted on exam, treatment is less likely to be beneficial.
- DECREASED PSYCHOTROPIC MEDICATIONS
As a single intervention, psychotropic medication reduction has been shown to reduce falls. Patients should be encouraged to decrease their use of sleep aids, including over-the-counter medications containing diphenhydramine or other sedating antihistamines. If a sedative-hypnotic is needed, a short-acting agent is preferred, and the dose should be started at about half of the usual starting adult dose. However, short-acting benzodiazepines, as well as the nonbenzodiazepine agent zolpidem have been associated with falls.
Antidepressants are associated with falls in a dose-dependent manner. Antidepressant and antipsychotic medication dose should be titrated downward if possible. Use of first-generation tricyclic antidepressants should be avoided.
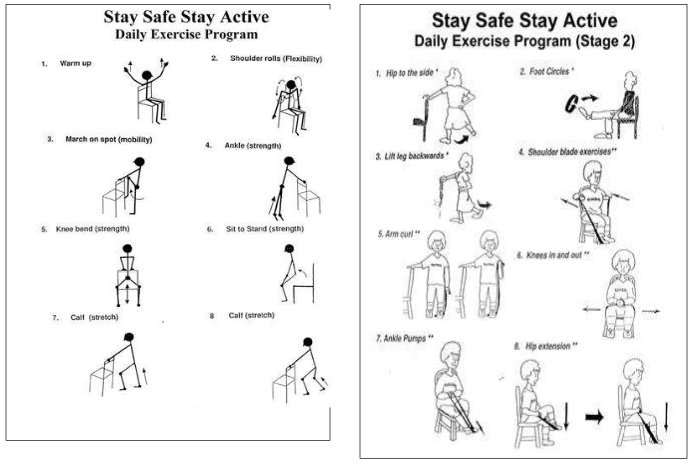
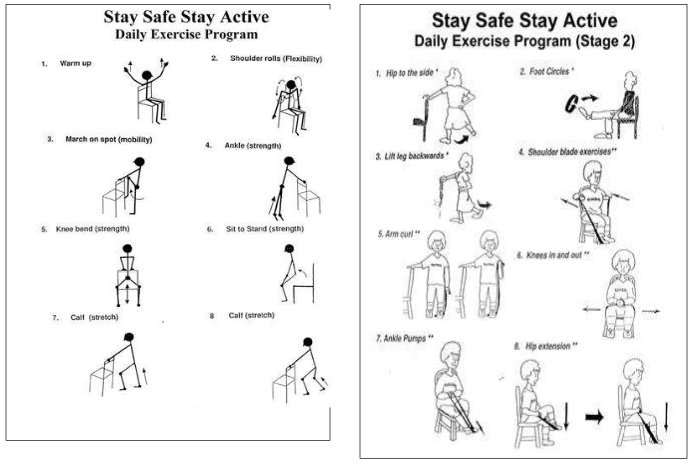
IMPLEMENTATION OF EXERCISE PROGRAM
Exercise training has been shown to positively improve balance, strength, flexibility and co-ordination among older people at risk of falling. Consequently, exercise has become a widely studied fall prevention intervention. Different exercise models have been evaluated, including group and individualized home programs among healthy and impaired populations. Many exercise models were tried for fall prevention as balance exercises, strength training, flexibility (muscle and joint stretching techniques), tai chi, and cardiovascular, endurance, and fitness training.
Tai Chi is one of the few specific evidence-based balance exercise programs. Tai Chi is a gentle form of martial arts involving a series of slow, synchronized postures with a focus on controlled breathing. It is well tolerated by healthier older adults and has been shown to positively impact both falls and blood pressure.
Exercise for balance and gait dysfunction is often focused on deficits in functional activities such as stair climbing, stepping over obstacles, or turning the head while walking. Practice can include conditions with environmental stress such as walking on foam or sand to simulate uneven, compliant, or shifting surfaces. High-cost, high-tech balance training equipment (e.g., Balance Master) has not been shown to be more effective at preventing falls
FOOTWEAR MODIFICATIONS:
Shoes with lower, thicker heels are preferable. The sole of the shoe is important for fall risk, but both hard-soled and rubber-soled shoes have advantages and disadvantages.
Thick, rubber-soled shoes, like running shoes, could interfere with sensory input from the feet but provide good pressure distribution and shock absorption for persons with insensitive or painful feet. Leather-soled shoes are thinner and offer less friction against the walking surface. While they simultaneously increase sensation from the feet and reduce the risk of tripping in persons with shuffling gait, they also can increase the risk of slips.
VITAMIN D REPLACEMENT:
Vitamin D replacement for those who are deficient has been shown to decrease falls and improve body sway. Vitamin D supplementation has also been shown to improve functional status. Although a recommendation of 800 IU Vitamin D/day for older adults is reasonable, some patients may require higher doses to achieve a desired level of 25-OH vitamin D of > 32 ng/mL. It is recommended that elderly patients who have sustained a fall be nutritionally assessed and advised to consume a high protein diet with vitamin and