CHAPTER 5
Medicines To Treat Cancer Pain
There is more than one way to treat pain.
Your doctor prescribes medicine based on the kind of pain you have and how severe it is. In studies, these medicines have been shown to help control cancer pain.
Doctors use three main groups of drugs for pain: nonopioids, opioids, and other types. You may also hear the term analgesics used for these pain relievers. Some are stronger than others. It helps to know the different kinds of medicines, why and how they’re used, how you take them, and what side effects you might expect.
1. Nonopioids —for mild to moderate pain
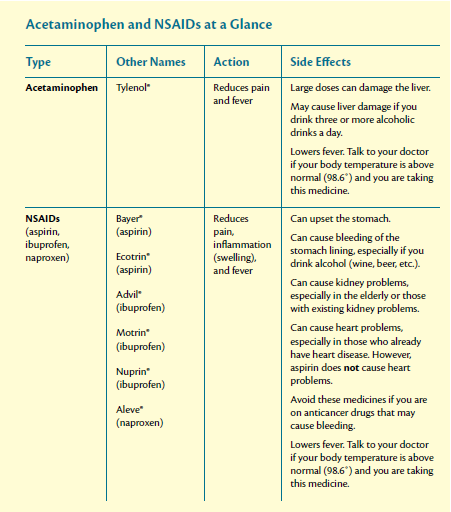
Nonopioids are drugs used to treat mild to moderate pain, fever, and swelling. On a scale of 0 to 10, a nonopioid may be used if you rate your pain from 1 to 4. These medicines are stronger than most people realize. In many cases, they are all you’ll need to relieve your pain. You just need to be sure to take them regularly.
You can buy most nonopioids without a prescription. But you still need to talk with your doctor before taking them. Some of them may have things added to them that you need to know about. And they do have side effects. Common ones, such as nausea, itching, or drowsiness, usually go away after a few days. Do not take more than the label says unless your doctor tells you to do so.
Nonopioids include:
-
Acetaminophen, which you may know as Tylenol®
Acetaminophen reduces pain. It is not helpful with inflammation. Most of the time, people don’t have side effects from a normal dose of acetaminophen. But taking large doses of this medicine every day for a long time can damage your liver. Drinking alcohol with the typical dose can also damage the liver. Make sure you tell the doctor that you’re taking acetaminophen. Sometimes it is used in other pain medicines, so you may not realize that you’re taking more than you should. Also, your doctor may not want you to take acetaminophen too often if you’re getting chemotherapy. The medicine can cover up a fever, hiding the fact that you might have an infection.
-
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (which you may know as Advil® or Motrin®) and aspirin
NSAIDs help control pain and inflammation. With NSAIDs, the most common side effect is stomach upset or indigestion, especially in older people. Eating food or drinking milk when you take these drugs may stop this from happening. NSAIDs may also keep blood from clotting the way it should. This means that it’s harder to stop bleeding after you’ve hurt yourself. NSAIDs can also sometimes cause bleeding in the stomach.
Tell your doctor if:
-
Your stools become darker than normal
-
You notice bleeding from your rectum
-
You have an upset stomach
-
You have heartburn symptoms
-
You cough up blood
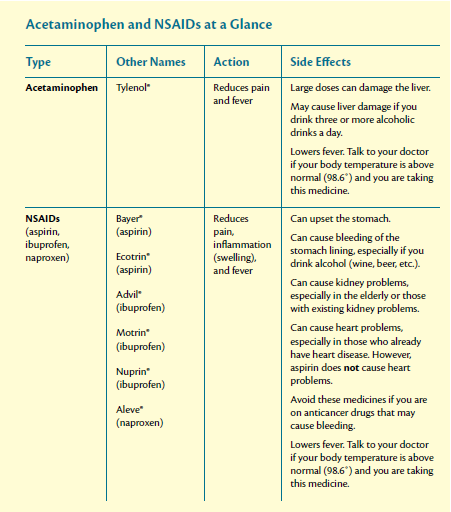
What to avoid when taking NSAIDs
Some people have conditions that NSAIDs can make worse. In general, you should avoid these drugs if you:
-
Are allergic to aspirin
-
Are getting chemotherapy
-
Are on steroid medicines
-
Have stomach ulcers or a history of ulcers, gout, or bleeding disorders
-
Are taking prescription medicines for arthritis
-
Have kidney problems
-
Have heart problems
-
Are planning surgery within a week
-
Are taking blood-thinning medicine (such as heparin or Coumadin®)
2. Opioids —for moderate to severe pain
If you’re having moderate to severe pain, your doctor may recommend that you take stronger drugs called opioids. Opioids are sometimes called narcotics. You must have a doctor’s prescription to take them. They are often taken with aspirin, ibuprofen, and acetaminophen.
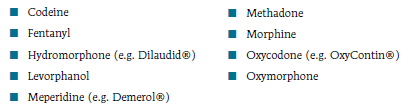
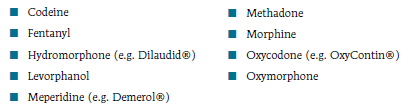
Common opioids include:
Getting relief with opioids
Over time, people who take opioids for pain sometimes find that they need to take larger doses to get relief. This is caused by more pain, the cancer getting worse, or medicine tolerance (see pages 20 and 21). When a medicine doesn’t give you enough pain relief, your doctor may increase the dose and how often you take it. He or she can also prescribe a stronger drug. Both methods are safe and effective under your doctor’s care. Do not increase the dose of medicine on your own.