APPENDIX C
FOOT CARE
Foot hygiene and sanitation are extremely important since feet are enclosed in heavy rigid footwear during most working hours and are constantly inaction. Foot care involves good hygiene measures such as bathing frequently, using foot powder, wearing properly fitted footwear to allow for ventilation, and correctly trimming toenails.
Section I
FOOT HYGIENE
The care of minor foot ailments should be given the utmost attention. Many major conditions requiring hospitalization and disability have resulted from neglected or maltreated minor conditions.
C-1. CONDITIONING
Conditioning is accomplished by progressively increasing the distance to be marched from day to day. Marching is a good way to strengthen the feet and legs; running alone will not suffice.
The arch, ankle, and calf can be conditioned by performing simple exercises—for example, rising high on the toes or placing the feet on towels and using the toes to roll the towel back under the arch.
C-2. PREVENTIVE MEASURES
Certain preventive measures can be implemented to avoid painful foot problems.
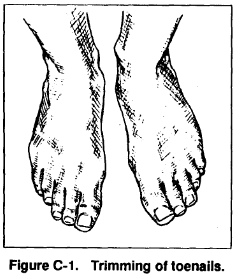
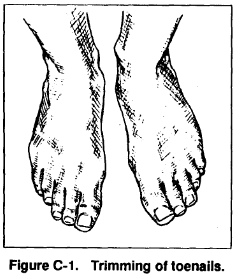
a. Before Marches. Trim toenails at least every two or three weeks, depending upon individual needs. Cut toenails short and square, and straight across (Figure C-1). Keep feet clean and dry, and use foot powder. Wear clean, dry, unmended, good-fitting socks (preferably cushion-soled) with seams and knots outside.
A nylon or polypropylene sock liner can reduce friction and add protection. Carry an extra pair of socks. Carefully fit new boots. When getting used to a new pair of boots, alternate with another pair; tape known hot spots before wearing.
b. During Halts. Lie down with the feet elevated during each halt. If time permits, massage the feet, apply foot powder, change socks, and medicate blisters. Cover open blisters, cuts, or abrasions with absorbent adhesive bandages. Obtain relief from swelling feet by slightly loosening bootlaces where they cross the arch of the foot.
c. After Marches. Repeat procedures for the care of feet, wash and dry socks, and dry boots. Medicate blisters, abrasions, corns, and calluses. Inspect painful feet for sprains and improper fitting of socks and boots. Feet can develop red, swollen, tender skin along the sides of the feet from prolonged marching, which could become blisters. Therefore, feet require aeration, elevation, rest, and wider footwear. Prevent major foot problems by keeping the feet clean. The formation of blisters and abrasions with dirt and perspiration can cause infection and serious injury.
If possible, give the feet a daily foot bath. In the field, cool water seems to reduce the sensation of heat and irritation. After washing, dry the feet well.
Section II
FOOT INJURIES
Many foot injuries can occur from foot marches, but only the most common are discussed herein.
C-3. BLISTERS AND ABRASIONS
Common causes of blisters and abrasions are improperly conditioned feet, ill-fitting footwear and socks, improperly maintained footwear, heat, and moisture. They are normally caused by friction or pressure, as opposed to impact.
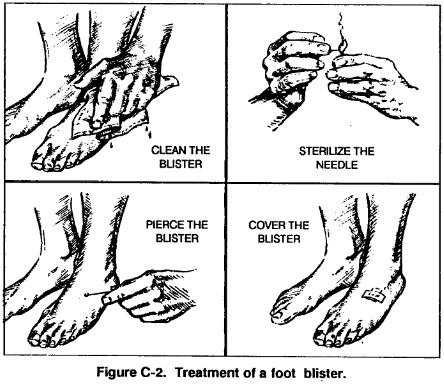
a. To clean a blister, wash gently around it with soap and water, being careful not to break the skin (Figure C-2). If unbroken, use a sterilized needle or knifepoint to prick the lower edge of the blister to remove fluid. (To sterilize needle or knifepoint, hold in a flame.) Do not remove the skin; cover the blister with an absorbent adhesive bandage or similar dressing, extending beyond the edge of the blister. After applying the dressing, dust the outside of the dressing and entire foot with foot powder.
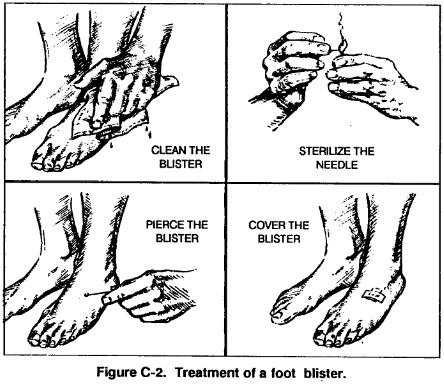
b. Use just enough foot power since it can harden and become irritating. Foot powder lessens friction on the skin and prevents the raw edges of the adhesive plaster from adhering to socks. The adhesive plaster should be smooth so it can serve as a “second skin.” Check the blister periodically for proper drying. After the blister has dried, remove the adhesive plaster.
Carefully inspect the foot for other problem areas that are red and tender that may need the protection of an adhesive plaster. Cover abrasions and cuts on the foot with absorbent adhesive bandages for rapid healing. In an emergency, medical personnel can inject tincture of benzoin into a blister to prevent further abrasion and loss of skin.
C-4. PERSPIRATION PROBLEMS
When feet perspire, the secretion decomposes and causes a foul odor. The skin between the toes usually becomes white and soft, rubs off easily, and is prone to abrasions. Treatment consists of washing and thoroughly drying the feet, and carefully painting the affected area with a cotton swab and the following solution
Formalin – one part
Rubbing alcohol – nine parts.
This solution should be allowed to dry. If the skin begins to burn, the excess solution should be washed off. It should be kept out of abrasions and cuts since it can cause severe pain. The entire area of the foot to include the ankle is painted. The areas around the heel and instep, and between toes should be treated since they are main trouble spots. The solution should be applied once daily until the perspiration is halted and the skin becomes hardened.
C-5. ATHLETE’S FOOT
Athlete’s foot usually occurs between the toes, on the sole of the foot, and at points of contact between skin and footwear. This and other mild chronic cases of fungus infection may respond to daily foot powder applications. If fungicidal ointment is available, it can be used in addition to foot powder. Ointment should be used as directed and while the feet are at rest. If applications of foot powder and ointment do not heal the infection, an aidman or surgeon should be consulted.
C-6. FROSTBITE
Frostbite is the freezing of a body part due to exposure to below-freezing temperatures, and it is classified as either superficial or deep. It is a constant hazard in operations performed at freezing temperatures, mainly when accompanied with strong winds. Normally, a cold sensation occurs that is followed by numbness and then a tingling, stinging, or aching, or even a cramping pain. The skin first turns red and then yellowish, pale gray, or waxy white.
a. Prevention of frostbite, or stopping it in its early stages, is easier than thawing and caring for frozen flesh.
Good-fitting clothing and properly worn equipment avoid interference with blood circulation, which could reduce the amount of heat delivered to the extremities. To prevent severe frostbite –
(1) Enough clothing must be worn for protection against cold and wind. The face must be protected during high winds and during exposure to aircraft propeller blast.
(2) Clothing and the body must be kept dry. To avoid perspiring when performing heavy work in the cold, soldiers should remove outer layers of clothing and then replace them when work is finished. Socks should be changed when the feet become moist.
(3) Cold metal should not be touched with the bare skin in extremely low temperatures. To do so could mean loss of skin.
(4) Adequate clothing and shelter must be provided during inactive times.
(5) The face, fingers, toes, and ears should be exercised or massaged to keep them warm and to detect any numb or hard areas.
(6) The buddy system should always be used. Soldiers should find partners and observe each other for signs of frostbite and for mutual aid if frostbite occurs. Any small frozen spots should be thawed immediately, using bare hands or other sources of body heat.
b. Some cases of frostbite may be superficial, which involves only the skin. If freezing extends below the skin, it demands more involved treatment to avoid or lessen the loss of the body part (fingers, toes, hands, or feet). Often there is no pain, so soldiers must observe each other for signs. Since it is difficult to distinguish between superficial and deep frostbite, a soldier should assume the injury to be deep and therefore serious. If numbness has been for a short time, the frostbite is probably superficial.
c. For treatment of superficial frostbite, the following measures must be adhered to:
(1) Cover cheeks with warm hands until the pain returns.
(2) Place uncovered frostbitten fingers under the opposing armpits next to the skin.
(3) Place bared frostbitten feet under clothing and against the chest of a companion.
(4) Do not rewarm by such measures as massage, exposure to open fires, cold-water soaks, or rubbing with snow.
(5) Be prepared for pain when thawing occurs.
d. For treatment of deep frostbite (freezing injury), the following measures must be adhered to:
(1) If freezing is considered deep, do not attempt to treat the injury in the field. This only causes increased pain and invites infection, greater damage, and even gangrene. Quickly evacuate injured personnel to a hospital or aid station.
(2) Protect the frozen body part from further injury and do not try to thaw it by rubbing, bending, or massaging.
(3) Do not rub body part with snow or place in cold or warm water; do not expose to hot air or open fires; and do not use ointments or poultices.
e. Soldiers should not walk on feet after thawing; it is safer to walk on frozen feet. However, thawing may occur spontaneously during transporting to a medical facility. This cannot be avoided since the entire body of the injured soldier must be kept warm.
f. Soldiers who have sustained any form of cold injury are more susceptible to a reoccurrence.
C-7. TRENCHFOOT
Trenchfoot is a thermal injury due to exposure to severe cold-weather conditions in a damp or wet environment in temperatures between 32 and 50 degrees F. Attributing causes include immobility of the limbs as in sitting or standing, insufficient clothing, and constriction of body parts due to boots, socks, and other garments.
a. Trenchfoot is similar to gradual frostbite since the primary causes are the same. The only difference is in the degree of cold. In the early stages of trenchfoot, feet and toes are pale, and they feel cold, numb, and stiff. Walking becomes labored. If preventive action is not taken at this stage, the feet will swell and become painful. In extreme cases of trenchfoot, the flesh dies and amputation of the foot or leg may be needed. Because the early stages of trenchfoot are not painful, soldiers must be alert to prevent it.
b. Socks and boots should be cleaned and dried daily, and feet should be dried soon after being wet. If soldiers must wear wet boots and socks, the feet should be exercised by wiggling the toes and bending the ankles, and they should be warmed with the hands. Then foot powder should be applied and dry socks put on.
c. In treating trenchfoot, the feet should be handled gently; they should not be rubbed or massaged. If needed, feet can be cleaned carefully with plain white soap and water, dried, elevated, and left exposed. While it is best to warm the patient, the feet should always be at room temperature. The patient should be carried and not allowed to walk on damaged feet.
C-8. IMMERSION FOOT
Immersion foot is a form of injury that follows prolonged immersion of the feet in water that is not cold enough to cause freezing or frostbite. It can occur after exposure in subtropical waters. Clinically and pathologically, immersion foot is like trenchfoot since its cause is the same – lowering the temperature of the body part involved. It is associated with dependency (legs and feet down as in sitting or standing) and immobility of the lower extremities, and with constriction of the limbs by clothing or shoes. Other important factors are: body cooling due to wind, total immersion, inadequate protective clothing, illness, and starvation. The treatment for immersion foot is the same as for trenchfoot.
C-9. STRESS FRACTURES AND MUSCLE INJURIES
Once stress fractures have occurred, they must be allowed time to heal. The affected area must rest for two or three weeks until the pain is gone, followed by a slow return to activity to avoid recurring injury. Personnel who have had an injury are more likely to be injured again. The best form of treatment for this type injury is prevention. This can be accomplished through a conditioning program and by ensuring major muscle groups are properly stretched and warmed up before marching.
Section III
CARE OF FOOTWEAR
Boots must be dried after use to avoid loosing shape and hardening of the leather. This can be done by placing a warm cloth in the boot or by any method that avoids rapid drying. To prevent moist leather from freezing during winter, boots should be placed inside a sleeping bag or used as a headrest.
C-10. BOOTS
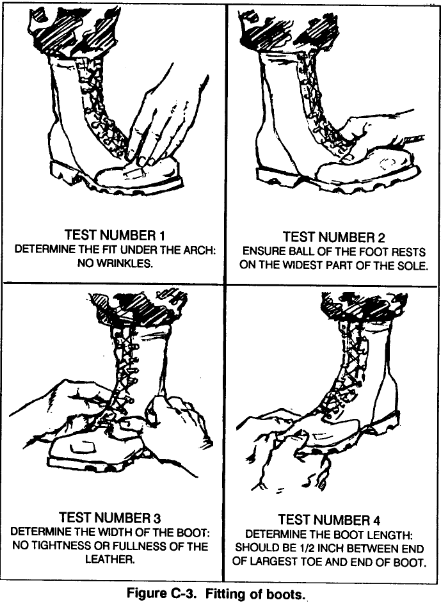
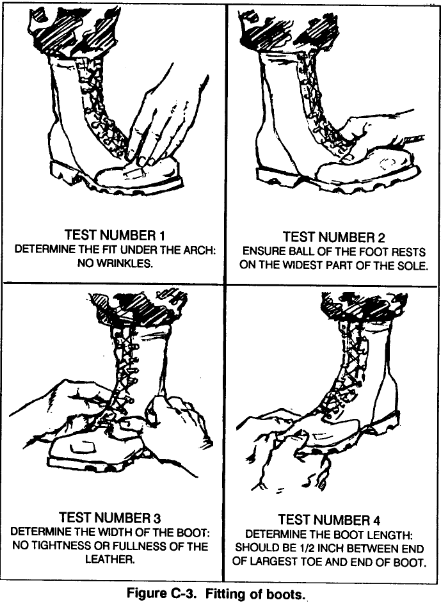
Two important factors in fitting boots are: the space between the end of the great toe and the toe of the boot should be the width of the thumb; and, in the unlaced boot, there should be enough space under the lower edge of the tongue to insert an index finger (Figure C-3).
C-9
a. Poorly fitted boots can cause blisters, abrasions, calluses, and corns. Pressure is caused by boots being too small; friction is caused by boots being too large. If the tops of the toes are involved, the cap is too low or too stiff. If the ends of the toes are affected, the boot is too short or too loosely laced. If the sides of the big and little toes become irritated, the boot is too narrow.
Irritation at the heel is caused by boots being too long, too loosely laced, or too wide a heel space.
b. Proper lacing of boots not only prevents blisters but also prevents improper blood flow in the foot. Laces can assume a seesaw action, which can produce along blister across the instep. To prevent blistering, lacing over the instep can be avoided. If possible, broad laces should be used and an extra pair should be carried.
C-11. SOCKS
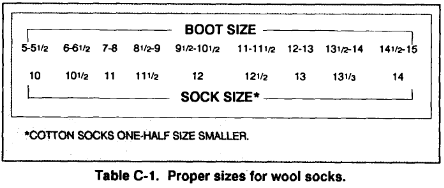
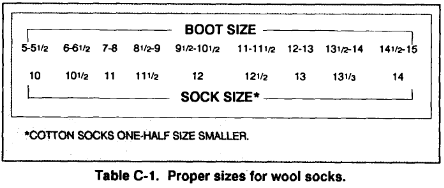
To check the fit of socks, a soldier should stand with his weight evenly distributed on both feet. If the socks fit correctly, no tightness or fullness should exist (Table C-1). The wool cushion-sole sock is best because it offers good foot protection.
a. Soldiers should allow 3/8 of an inch for shrinkage of new socks. Those that are too large wrinkle inside the shoe, rub the feet, and cause blisters and abrasions. Socks that are too small wear quickly and reduce blood flow in the foot. When wearing two pairs of socks, soldiers should wear an outer pair at least a half-size larger than usual. Socks must be changed daily–dirty socks are conductors of heat and allow warmth to escape. They should be washed in lukewarm water to preserve the fiber of the sock since hot water can cause them to shrink.
b. When socks become damp, they can be dried by placing them inside a shirt next to the body. Socks should be completely dry before wearing. If it is not possible to wash the socks, they should be changed; the dirty socks should be dried and kneaded with the hands to remove dirt and hardness.