PART
2
B
Wha r
t H ain
appens
to the
in AD

The
Hallmarks of AD
Alzheimer’s disease disrupts critical metabolic AMYLOID PLAQUES
processes that keep neurons healthy. These Amyloid plaques are found in the spaces between disruptions cause nerve cells in the brain the brain’s nerve cells. They were first described to stop working, lose connections with by Dr. Alois Alzheimer in 1906. Plaques consist other nerve cells, and finally die. The destruction
of largely insoluble deposits of an apparently toxic
and death of nerve cells causes the memory failure, protein peptide, or fragment, called beta-amyloid.
personality changes, problems in carrying out
We now know that some people develop
daily activities, and other features of the disease.
some plaques in their brain tissue as they age.
The brains of people with AD have an abundance However, the AD brain has many more plaques of two abnormal structures—amyloid plaques
in particular brain regions. We still do not know
and neurofibrillary tangles—that are made of
whether amyloid plaques themselves cause AD or
misfolded proteins (see Protein Misfolding on
whether they are a by-product of the AD process.
page 41 for more information). This is especially
We do know that genetic mutations can increase
true in certain regions of the brain that are
production of beta-amyloid and can cause rare,
important in memory.
inherited forms of AD (see Genes and Early-
The third main feature of AD is the loss of
Onset Alzheimer’s Disease on page 38 for
connections between cells. This leads to dimin-
more on inherited AD).
ished cell function and cell death.
To view a video showing what happens to
the brain in AD, go to www.nia.nih.gov/
alzheimers/alzheimers-disease-video.
ALZHEIMER’S DISEASE Unraveling the Mystery 21
P A R T 2 What Happens to the Brain in AD
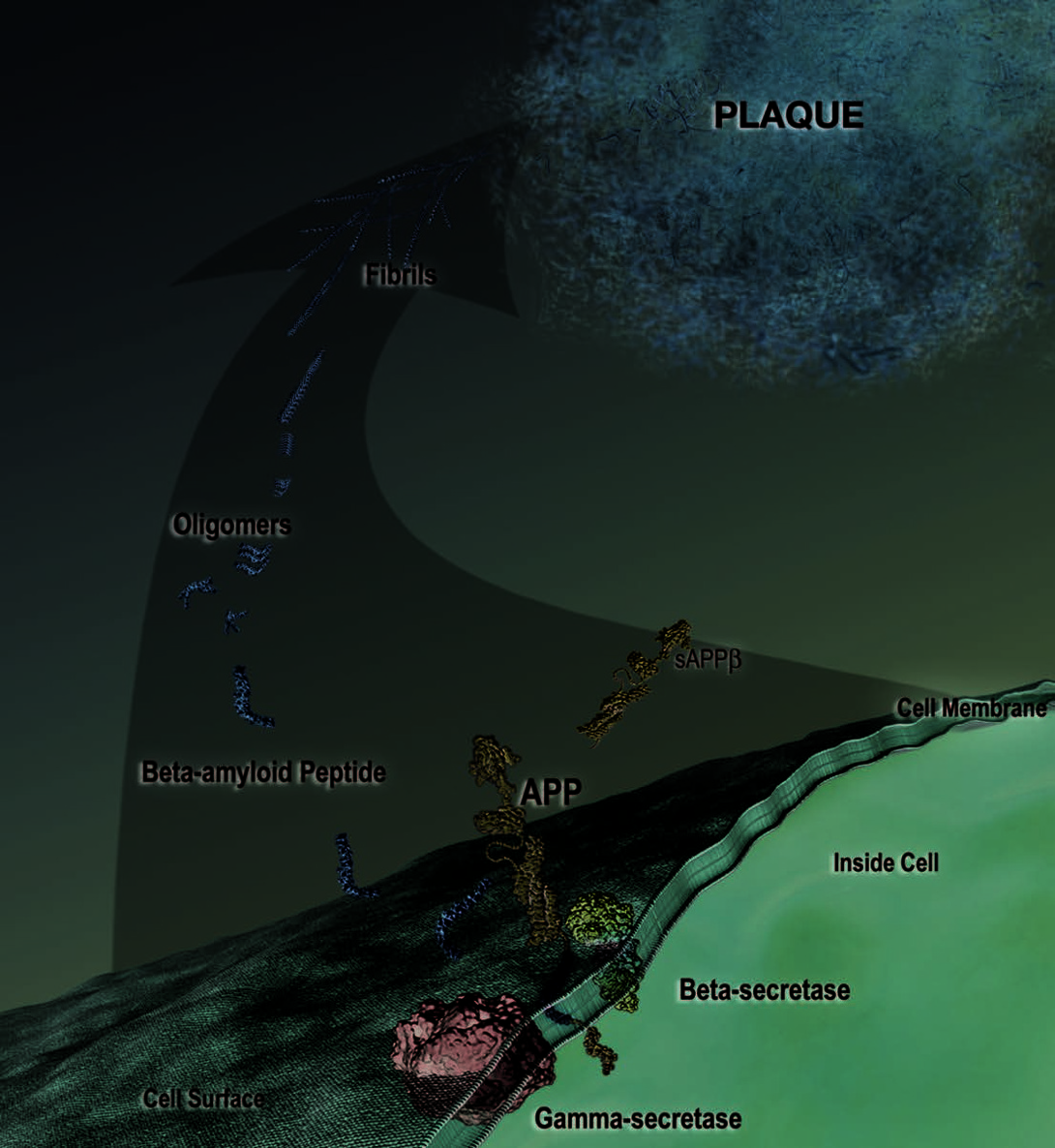
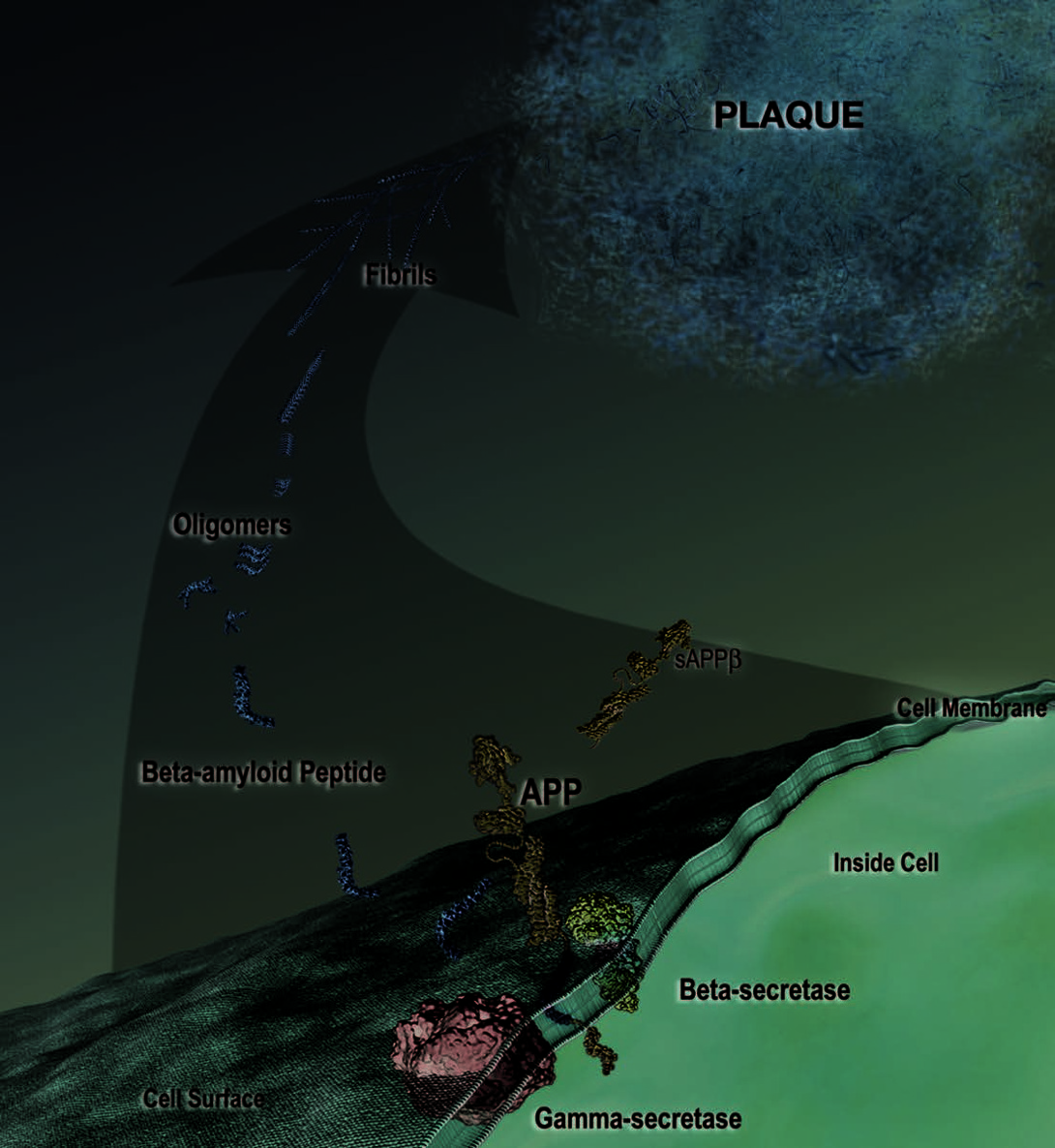
From APP to Beta-Amyloid Plaques
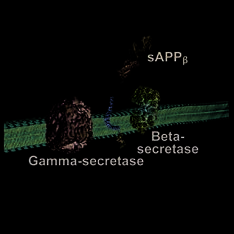
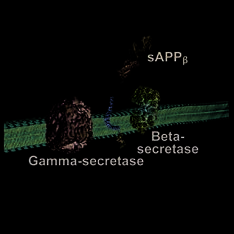
the APP molecule at one
end of the beta-amyloid
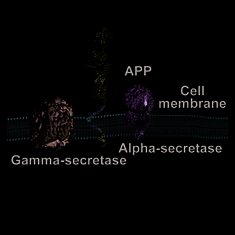
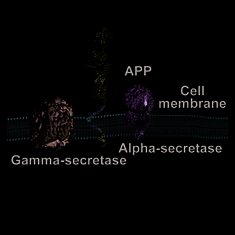
Amyloid precursor protein (APP), the starting
point for amyloid plaques, is one of many proteins
associated with the cell membrane, the barrier that
peptide, releasing sAPPβ
encloses the cell. As it is being made inside the cell,
from the cell (Figure 3).
APP becomes embedded in the membrane, like a tooth-
Gamma-secretase then
pick stuck through the skin of an orange (Figure 1).
cuts the resulting APP
In a number of cell com-
fragment, still tethered in
Figure 3
partments, including the
the neuron’s membrane,
outermost cell membrane,
at the other end of the
specific enzymes snip, or
beta-amyloid pep tide.
cleave, APP into discrete
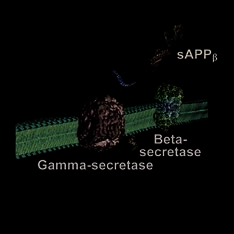
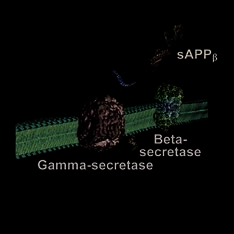
Following the cleavages
fragments. In 1999 and
at each end, the beta-
2000, scientists identified
amyloid peptide is
Figure 1
the enzymes responsible for
released into the space
cleaving APP. These enzymes are called alpha-
outside the neuron and
Figure 4
secretase, beta-secretase, and gamma-secretase.
begins to stick to other
In a major breakthrough, scientists then discov ered
beta-amyloid peptides (Figure 4). These small,
that, depending on which enzyme is involved and
soluble aggregates of two, three, four, or even
the segment of APP where the cleaving occurs, APP
up to a dozen beta-amyloid peptides are called
processing can follow one of two pathways that
oligomers. Specific sizes of oligomers may
have very different consequences for the cell.
be responsible for reacting with receptors on
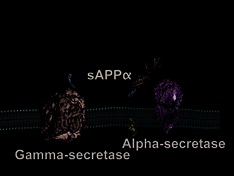
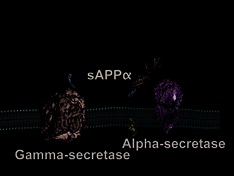
In the benign pathway, alpha-secretase cleaves the
neighboring cells and synapses, affecting their
APP molecule within the portion that has the potential to ability to function.
become beta-amyloid. This eliminates the production of
It is likely that some oligomers are cleared from
the beta-amyloid peptide and the potential for plaque
the brain. Those that cannot be cleared clump
buildup. The cleavage releases from the neuron a frag-
together with more beta-amyloid peptides. As the
ment called sAPPα, which has beneficial prop erties,
process continues, oligomers grow larger, becoming
such as promoting neuronal growth and survival. The
entities called protofibrils and fibrils. Eventually, other remaining APP fragment, still tethered in the neuron’s
proteins and cellular material are added, and these
membrane, is then cleaved by gamma-secretase at
increasingly insoluble entities combine to become the
the end of the beta-amyloid segment. The smaller of
well-known plaques that are characteristic of AD.
the resulting fragments also is released into the space
For many years, scientists thought that plaques
outside the neuron, while
might cause all of the damage to neurons that is seen
the larger fragment remains
in AD. However, that concept has evolved greatly
within the neuron and
in the past few years. Many scientists now think that
interacts with factors in the
oligomers may be a major culprit. Many scientists
nucleus (Figure 2).
also think that plaques actually may be a late-stage
In the harmful pathway, attempt by the brain to get this harmful beta-amyloid beta-secretase first cleaves away from neurons.
Figure 2
22 ALZHEIMER’S DISEASE Unraveling the Mystery
From APP to Beta-Amyloid Plaque
ALZHEIMER’S DISEASE Unraveling the Mystery 23
P A R T 2 What Happens to the Brain in AD
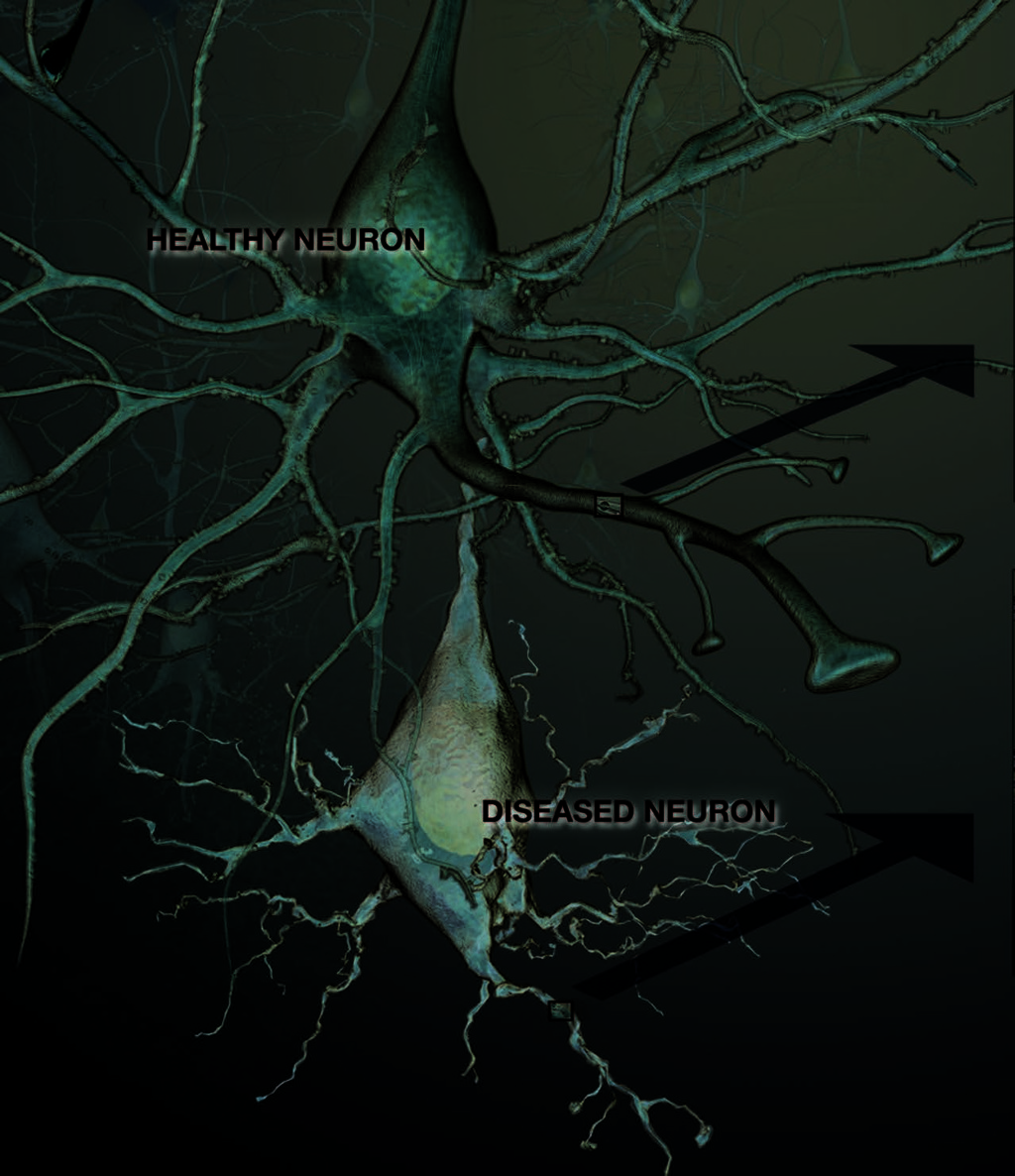
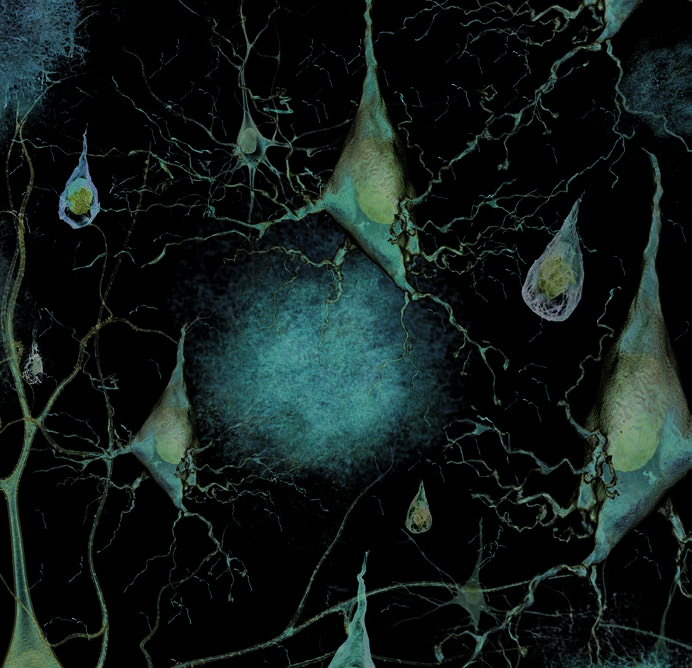
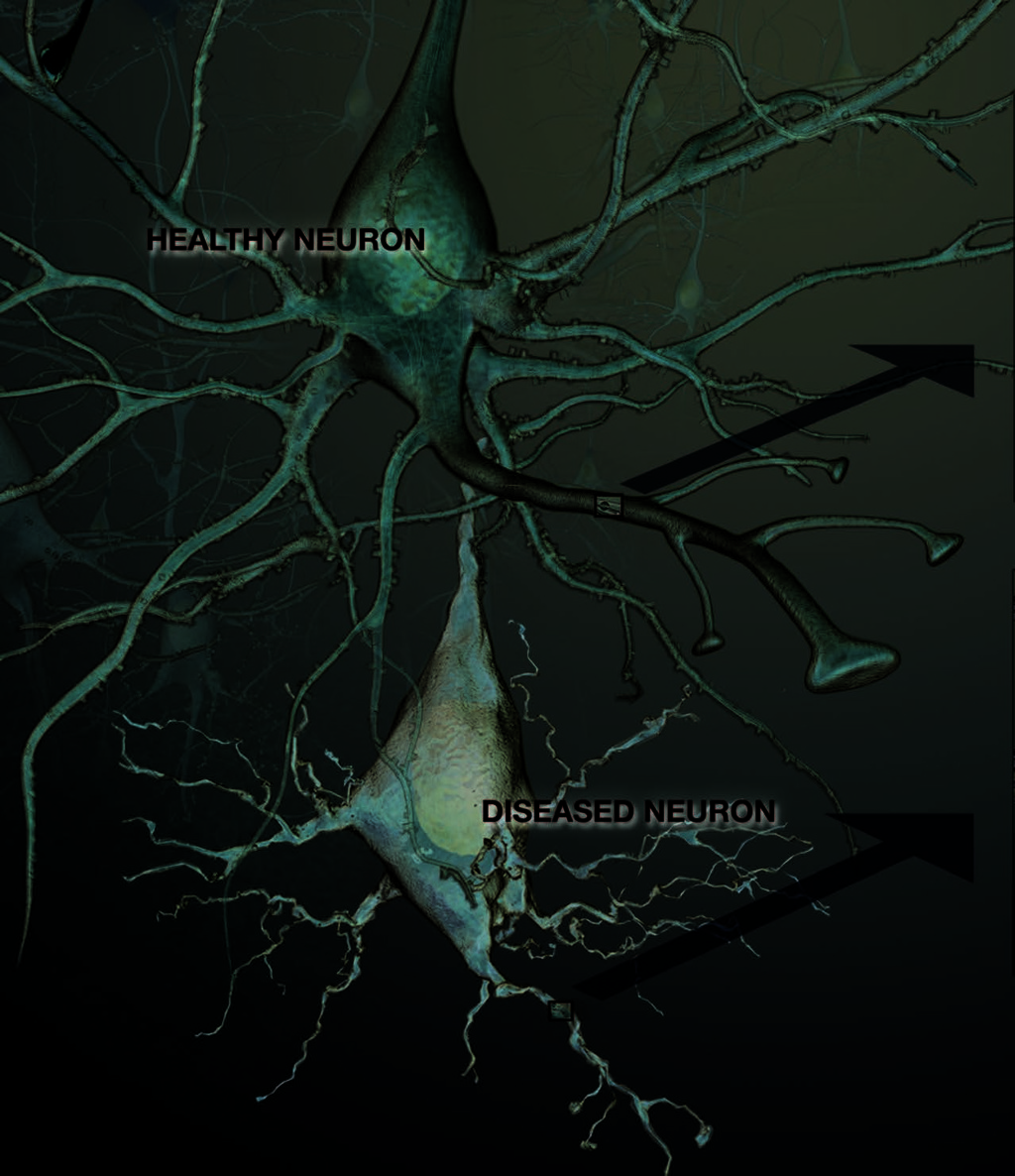
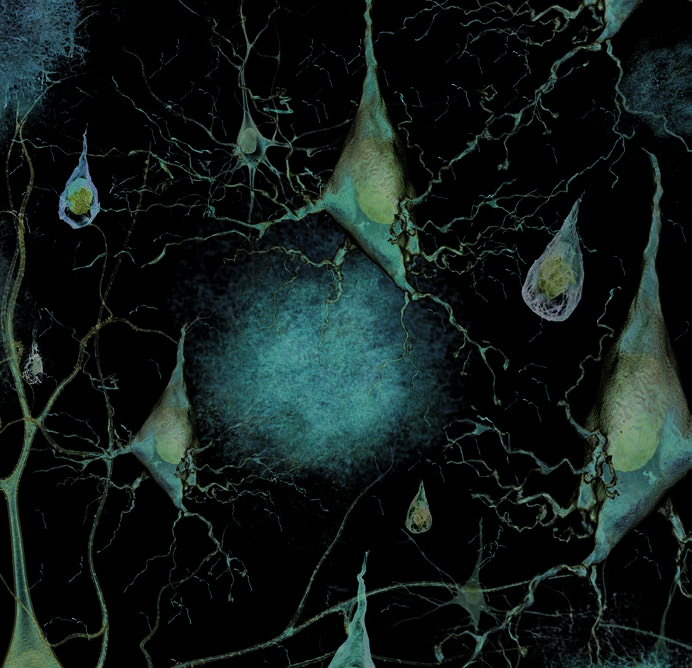
Healthy and Diseased Neurons
24
24 ALZHEIMER’S DISEASE Unraveling the Mystery
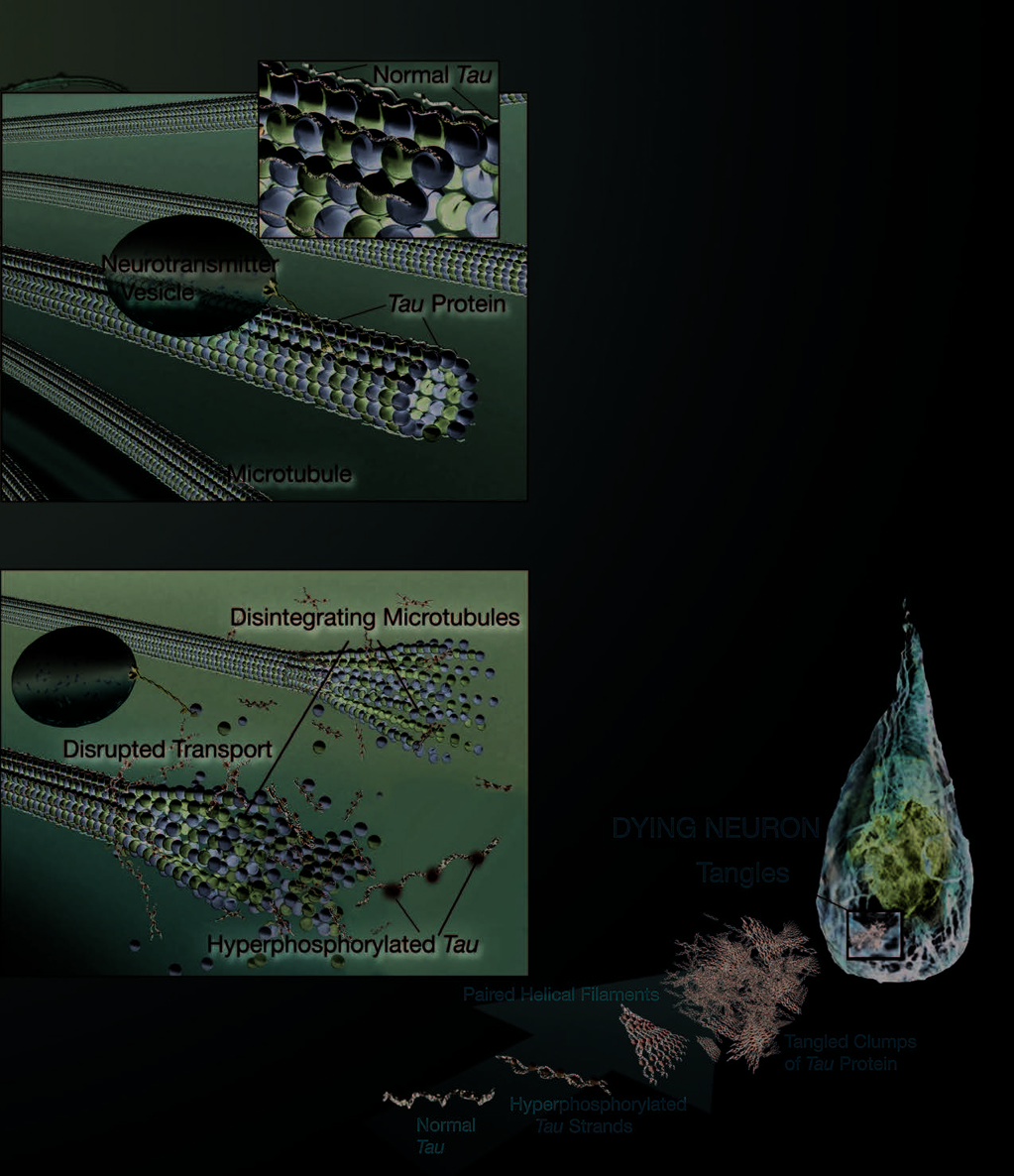


Inside a
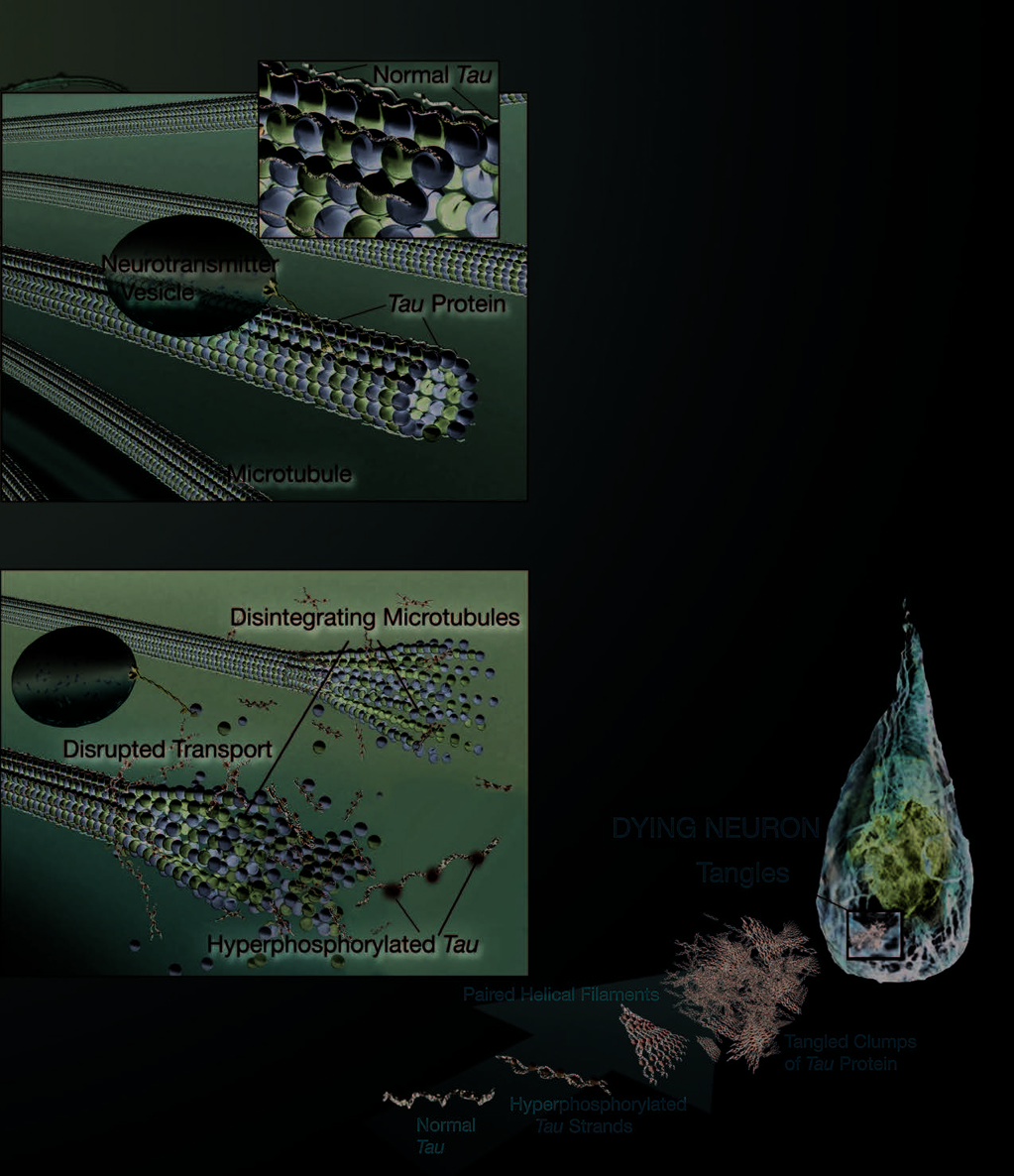
NEUROFIBRILLARY TANGLES
Healthy Neuron
The second hallmark of AD, also described by
Dr. Alzheimer, is neurofibrillary tangles. Tangles
are abnormal collections of twisted protein
threads found inside nerve cells. The chief
component of tangles is a protein called tau.
Healthy neurons are internally supported
in part by structures called microtubules,
which help transport nutrients and other
cellular components, such as neurotransmitter-
containing vesicles, from the cell body
down the axon.
Tau, which usually has a certain number of
phosphate molecules attached to it, binds to
microtubules and appears to stabilize them. In
AD, an abnormally large number of additional
phosphate molecules attach to tau. As a result
of this “hyperphosphorylation,” tau disengages
from the microtubules and begins to come
together with other tau threads. These tau
Inside a Diseased Neuron
threads form structures called paired helical
filaments, which can become enmeshed
with one another, forming tangles
within the cell. The microtubules can
disintegrate in the process, collaps-
ing the neuron’s internal transport
network. This collapse damages
the ability of neurons to com-
municate with each other.
Formation of Tau Tangles
ALZHEIMER’S DISEASE Unraveling the Mystery 25
25

P A R T 2 What Happens to the Brain in AD
LOSS OF CONNECTION BETWEEN
The AD process not only inhibits communi-
CELLS AND CELL DEATH
cation between neurons but can also damage
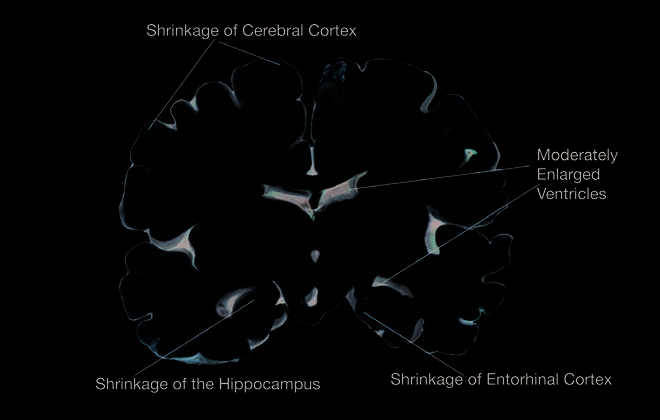
The third major feature of AD is the gradual
neurons to the point that they cannot function
loss of connections between neurons. Neurons
prop erly and eventually die. As neurons die
live to communicate with each other, and this
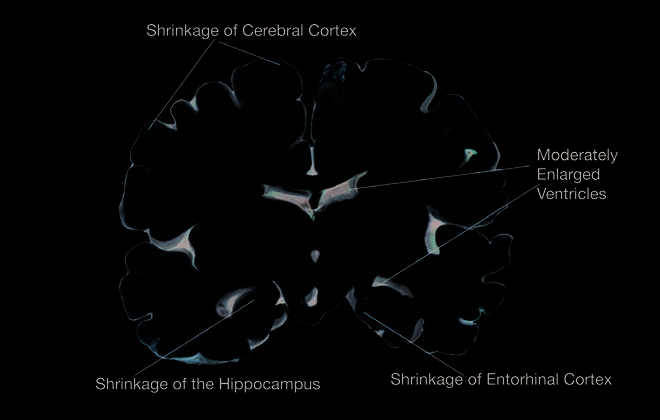
throughout the brain, affected regions begin to
vital function takes place at the synapse. Since
shrink in a process called brain atrophy. By the
the 1980s, new knowledge about plaques and
final stage of AD, damage is widespread, and
tangles has provided important insights into
brain tissue has shrunk significantly.
their possible damage to synapses and on the
development of AD.
Loss of Connection
Between Cells
This illustration shows
the damage caused by AD:
plaques, tangles, and the
loss of connection between
neurons.
26 ALZHEIMER’S DISEASE Unraveling the Mystery
Changing Brain
The
in AD
No one knows exactly what starts severity of cognitive problems at diagnosis.
the AD process or why some of the
Although the course of the disease is not the same
normal changes associated with
in every person with AD, symptoms seem to
aging become so much more extreme develop over the same general stages.
and destructive in people with the disease. We
know a lot, however, about what happens in the
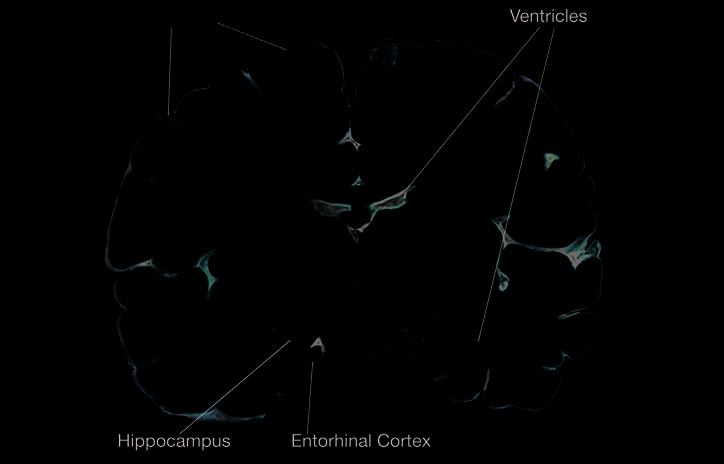
PRECLINICAL AD
brain once AD takes hold and about the physical
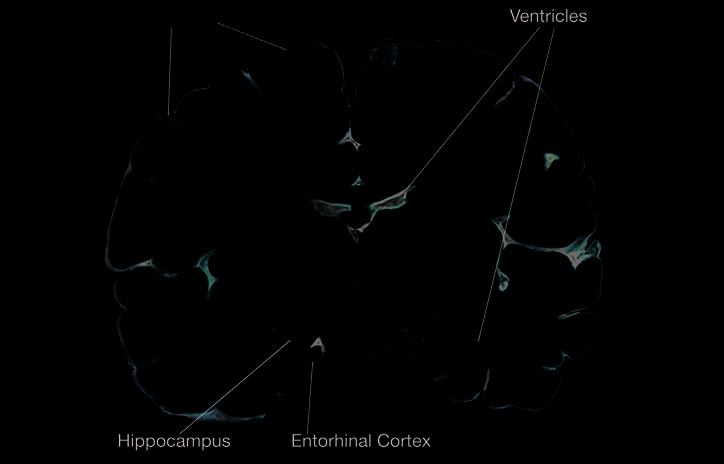
AD begins deep in the brain, in the entorhinal
and mental changes that occur over time. The
cortex, a brain region that is near the hippocampus
time from diagnosis to death varies—as little as
and has direct connections to it. Healthy neurons
3 or 4 years if the person is older than 80 when
in this region begin to work less efficiently, lose
diagnosed to as long as 10 or more years if the
their ability to communicate, and ultimately die.
person is younger. Several other factors besides
This process gradually spreads to the hippocam-
age also affect how long a person will live with
pus, the brain region that plays a major role in
AD. These factors include the person’s sex,
learning and is involved in converting short-term
the presence of other health problems, and the
memories to long-term memories. Affected
regions begin to atrophy. Ventricles, the fluid-
filled spaces inside the brain, begin to enlarge
Preclinical AD
as the process continues.
Scientists believe that these brain changes
begin 10 to 20 years before any clinically
detectable signs or symptoms of forgetful-
ness appear. That’s why they are increasingly
interested in the very early stages of the disease
process. They hope to learn more about what
happens in the brain that sets a person on the
path to developing AD. By knowing more about
the early stages, they also hope to be able to
ALZHEIMER’S DISEASE Unraveling the Mystery 27
P A R T 2 What Happens to the Brain in AD
PiB and PET
Imagine being able to see deep inside the brain tissue of
a living person. If you could do that, you could find out
whether the AD process was happening many years before
symptoms were evident. This knowledge could have a
profound impact on improving early diagnosis, monitoring
disease progression, and tracking response to treatment.
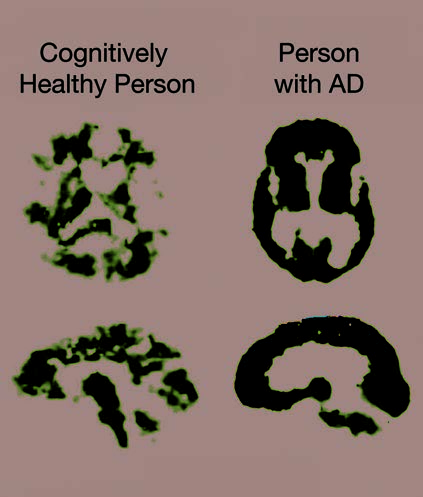
Scientists have stepped closer to this possibility with the development of a radiolabeled compound called Pittsburgh
Compound B (PiB). PiB binds to beta-amyloid plaques in the
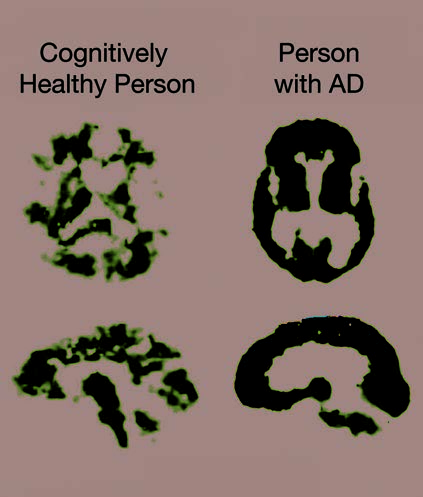
brain and it can be imaged using PET scans. Initial studies showed that people with AD take up more PiB in their brains than do cognitively healthy older people. Since then, scientists have found high levels of PiB in some cognitively healthy people, suggesting that the damage from beta-amyloid may In this PET scan, the red and yellow colors already be underway. The next step will be to follow these
indicate that PiB uptake is higher in the brain
cognitively healthy people who have high PiB levels to see
of the person with AD than in the cognitively
whether they do, in fact, develop AD over time.
healthy person.
develop drugs or other treatments that will
to a substance, the presence of a disease, or the
slow or stop the disease process before significant progression over time of a disease. For example, impairment occurs (see The Search for New
high blood cholesterol is a biomarker for risk of
Treatments on page 54 for more information).
heart disease. Such tools are critical to helping
scientists detect and understand the very early
VERY EARLY SIGNS AND SYMPTOMS
signs and symptoms of AD.
At some point, the damage occurring in the brain
begins to show itself in very early clinical signs and Mild Cognitive Impairment symptoms. Much research is being done to identify As some people grow older, they develop memory these early changes, which may be useful in
problems greater than those expected for their age.
predicting dementia or AD. An important part of
But they do not experience the personality changes
this research effort is the development of increas-
or other problems that are characteristic of AD.
ingly sophisticated neuroimaging techniques (see
These people may have a condition called mild
Exciting New Developments in AD Diagnosis
cognitive impairment (MCI). MCI has several
on page 50 for more on neuroimaging) and the use subtypes. The type most associated with memory of biomarkers. Biomarkers are indicators, such as
loss is called amnestic MCI. People with MCI are
changes in sensory abilities, or substances that ap-
a critically important group for research because
pear in body fluids, such as blood, cerebrospinal
fluid, or urine. Biomarkers can indicate exposure
28 ALZHEIMER’S DISEASE Unraveling the Mystery
Charting the Course from Healthy Aging to AD
This chart shows cur-
Amnestic MCI:
Cognitive
rent thinking about the
AD brain
memory problems;
decline
evolution from healthy aging
changes start
other cognitive
accelerates
to AD. Researchers view it as
decades before
functions OK;
after AD
a series of events that occur
symptoms
brain compensates
diagnosis
show
for changes
in the brain over many years.
This gradual process, which
results from the combination of
biological, genetic, environ-
Normal age-related
mental, and lifestyle factors,
memory loss
eventually sets some people
Total loss of
on a course to MCI and
independent
possibly AD. Other people,
function
whose genetic makeup may
be the same or different and
who experience a different
Birth 40
60
80 Death
combination of factors over a
Life Course lifetime, continue on a course
Healthy Aging
Amnestic MCI
Clinically Diagnosed AD
of healthy cognitive aging.
a much higher percentage of them go on to de-
AD (see Genetic Factors at Work in AD on
velop AD than do people without these memory
page 36 for more information). And, they have
problems. About 8 of every 10 people who fit the
found that different brain regions appear to
definition of amnestic MCI go on to develop AD
be activated during certain mental activities in
within 7 years. In contrast, 1 to 3 percent of peo-
cognitively healthy people and those with MCI.
ple older than 65 who have normal cognition will These changes appear to be related to the early develop AD in any one year.
stages of cognitive impairment.
However, researchers are not yet able to say
definitively why some people with amnestic MCI
Other Signs of Early AD Development
do not progress to AD, nor can they say who
As scientists have sharpened their focus on the
will or will not go on to develop AD. This raises
early stages of AD, they have begun to see hints of
pressing questions, such as: In cases when MCI
other changes that may signal a developing disease
progresses to AD, what was happening in the brain process. For example, in the Religious Orders Study, that made that transition possible? Can MCI be
a large AD research effort that involves older nuns,
prevented or its progress to AD delayed?
priests, and religious brothers, investigators have
Scientists also have found that genetic
factors may play a role in MCI, as they do in
ALZHEIMER’S DISEASE Unraveling the Mystery 29
P A R T 2 What Happens to the Brain in AD
explored whether changes in older adults’ ability to
Mild to Moderate AD
move about and use their bodies might be a sign of
early AD. The researchers found that participants
with MCI had more movement difficulties than the
cognitively healthy participants but less than those
with AD. Moreover, those with MCI who had lots
of trouble moving their legs and feet were more
than twice as likely to develop AD as those with
good lower body function.
It is not yet clear why people with MCI might
have these motor function problems, but the
scientists who conducted the study speculate that
they may be a sign that damage to blood vessels in
the brain or damage from AD is accumulating in
areas of the brain responsible for motor function.
If further research shows that some people with
MCI do have motor function problems in addi-
MILD AD
tion to memory problems, the degree of difficulty, As AD spreads through the brain, the number of especially with walking, may help identify those at plaques and tangles grows, shrinkage progresses, risk of progressing to AD.
and more and more of the cerebral cortex is
Other scientists have focused on changes in
affected. Memory loss continues and changes
sensory abilities as possible indicators of early
in other cognitive abilities begin to emerge. The
cognitive problems. For example, in one study they clinical diagnosis of AD is usually made during found associations between a decline in the ability
this stage. Signs of mild AD can include:
to detect odors and cognitive problems or dementia.
These findings are tentative, but they are
■ Memory loss
promising because they suggest that, some day, it
■ Confusion about the location of familiar places
may be possible to develop ways to improve early
(getting lost begins to occur)
detection of MCI or AD. These tools also will help ■ Taking longer than before to accomplish scientists answer questions about causes and very
normal daily tasks
early development of AD, track changes in brain
■ Trouble handling money and paying bills
and cognitive function over time, and ultimately
■ Poor judgment leading to bad decisions
track a person’s response to treatment for AD.
■ Loss of spontaneity and sense of initiative
■ Mood and personality changes, increased
anxiety and/or aggression
In mild AD, a person may seem to be healthy
but is actually having more and more trouble
making sense of the world around him or her. The
realization that something is wrong often comes
gradually to the person and his or her family.
30 ALZHEIMER’S DISEASE Unraveling the Mystery
Accepting these signs as something other than
■ Hallucinations, delusions, suspiciousness or
normal and deciding to go for diagnostic tests can
paranoia, irritability
be a big hurdle for people and families. Once this
■ Loss of impulse control (shown through
hurdle is overcome, many families are relieved to
undressing at inappropriate times or places
know what is causing the problems. They also can
or vulgar language)
take comfort in the fact that despite a diagnosis
■ An inability to carry out activities that involve
of MCI or early AD, a person can still make
multiple steps in sequence, such as dressing,
meaningful contributions to his or her family
making a pot of coffee, or setting the table
and to society for a time.
<