Frailty in Older Persons
Frailty can be defined as an age-associated declines in physiologic reserve and function across multi-organ systems, leading to increased vulnerability for adverse health outcomes.
Clinical implications of frailty:
- It is a warning sign for high risk of adverse health outcomes.
- The explanation for downward spiral in many elderly patients after acute illness.
- Frailty has been widely utilized as a mortality risk assessment tool. Reflects biological age that predicts mortality better than chronological age.
- Frailty is often described as a transitional phase between successful ageing and disability.
- Frail elderly need specific management: Regardless of age, a frail person may be unable to withstand aggressive medical treatment that could benefit a nonfrail person.
Epidemiology:
- Although exact definitions and screening methods vary, approximately 15 % of the US population over age 65 and living in the community are considered frail.
- In 15 studies that included 44,894 participants identified a prevalence of frailty of 9.9 %; when psychosocial aspects were included in the definition, prevalence was 13.6 % among eight studies that included 24,072 participants.
- Prefrail individuals, generally identified with a physical frailty type tool , are more common in these population studies, with prevalence ranging from 28 to 44 %.
- Of those individuals who were prefrail, over 10 % went on to become frail over the next 3 years.
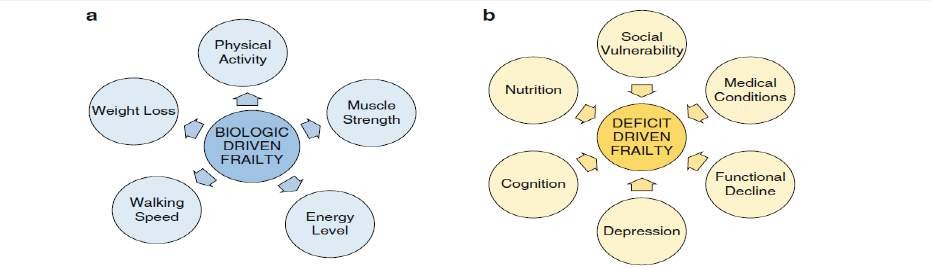
The biology of frailty is explained by two models:
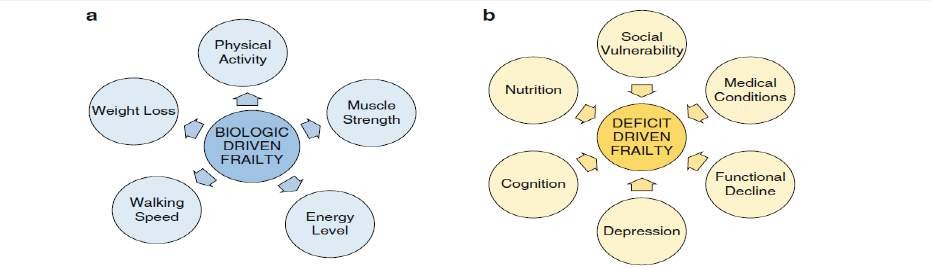
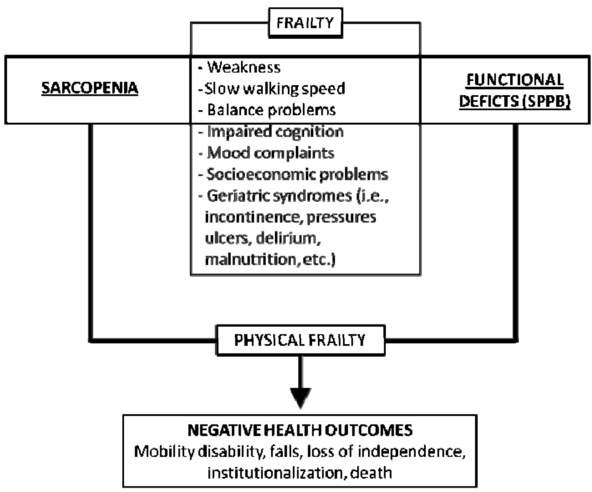
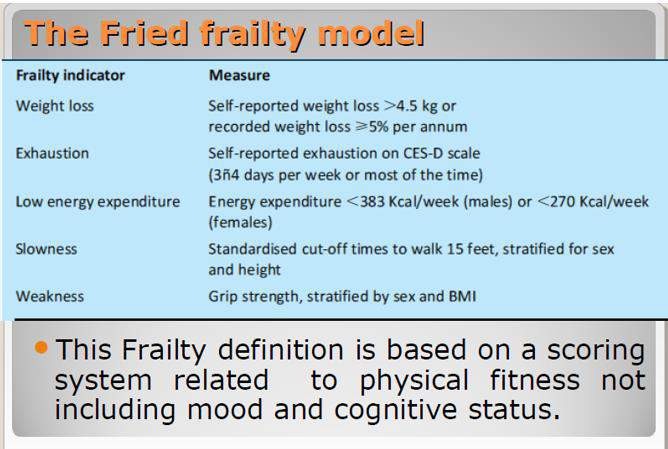
1. Phenotypic frailty
- A cycle of physiological decline was hypothesized that included interrelated and reinforcing declines in metabolism, nutrition utilization, and skeletal muscle that in sum drove worsening vulnerability.
- Triggers of this cycle of decline included acute illnesses, some medications, and aging related biological changes in genetic predisposed elderly.
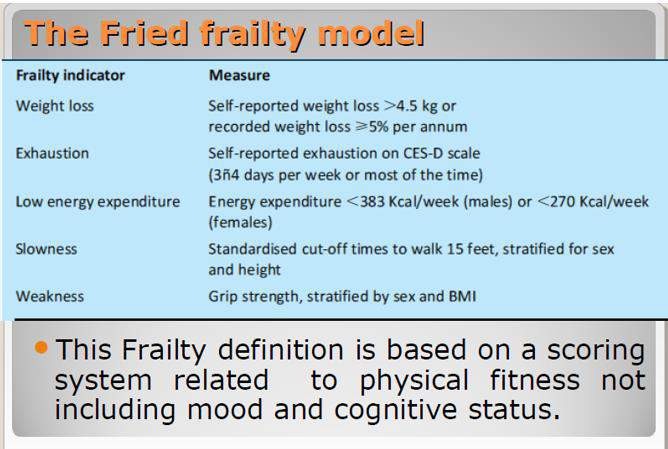
- These physiological impairments result in the five clinical characteristics of frailty: weakness, low energy, slow walking speed, low physical activity and weight loss.(Fried criteria for frailty diagnosis)
- The presence of any three of these phenotypes indicates that a person is ‘frail’; one or two phenotypes indicate that the person is ‘prefrail’ and absence of these characteristics indicates the person is ‘robust’.
2. Deficit-driven frailty
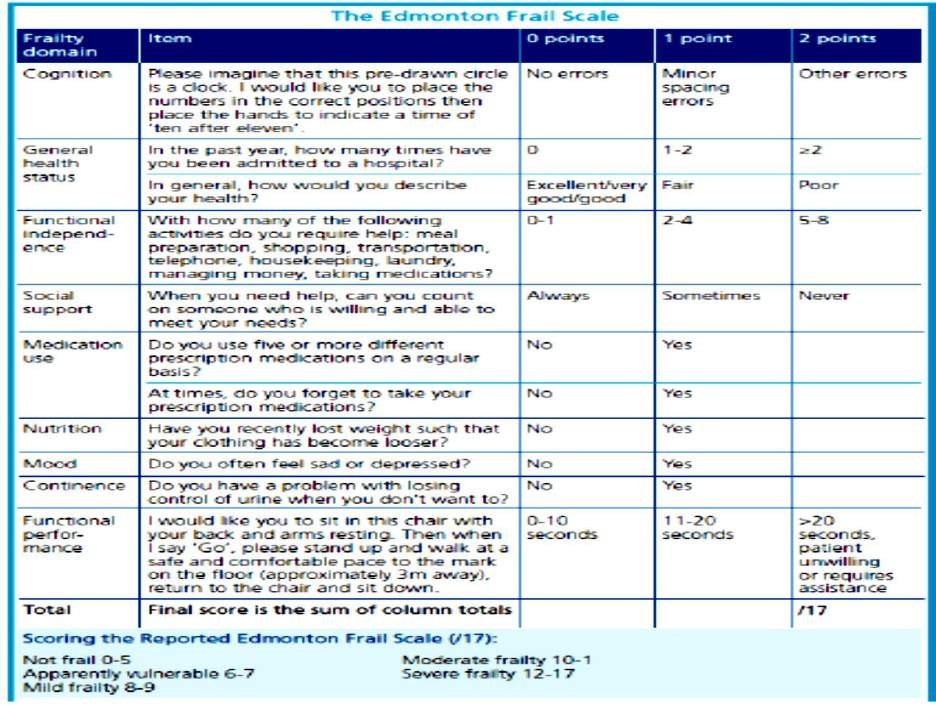
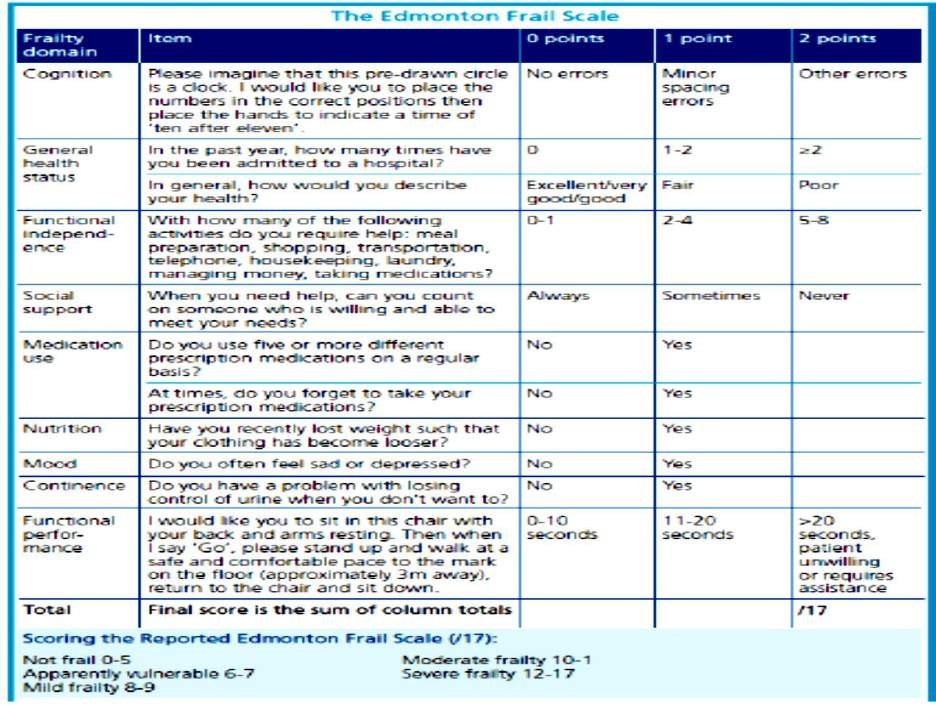
- Frailty as an aggregate of illnesses, disability measures, cognitive and functional declines that has been termed deficit-driven frailty. According to this model, the more deficits or conditions that an individual has, the more frail the individual is.
- In this diagnostic approach, almost any conditions or deficits are interchangeable in index tools.
- This conceptual basis has also been widely utilized to develop risk assessment tools that tally a broad range of comorbid illnesses, mobility and cognitive measures, and environmental factors to capture frailty.
Initiators
(triggers)
of frailty:
|
Aging
|
Genetics
|
|
Environmental factors (UVR, Pollution),
Drugs
|
Internal stressors (inflammatory, malignancy, malnutrition)
|
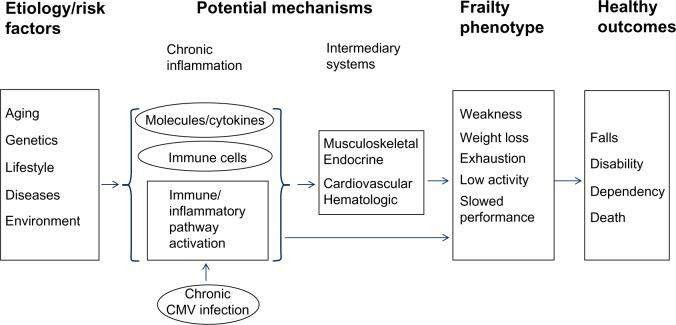
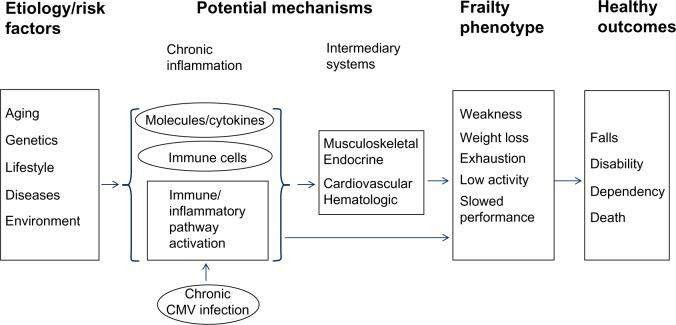
The mechanisms of frailty
|
Chronic inflammatory pathway activation
|
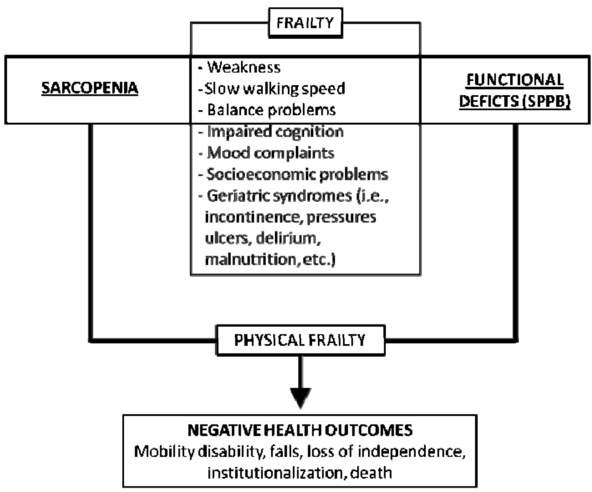
Decline in skeletal muscle function and mass(Sarcopenia)
|
Endocrinal changes contribute to frailty
|
- Serum levels of the proinflammatory cytokine IL-6 and C-reactive protein (CRP), as well as white blood cell and monocyte counts, are elevated in frail older adults.
- IL-6 acts as a transcription factor and signal transducer that adversely impacts skeletal muscle, appetite, adaptive immune system function, and cognition and contributes to anemia.
- Immune system activation may trigger the clotting cascade, with a demonstrated association between frailty and clotting markers (factor VIII, fibrinogen, and D-dimer).
- there is evidence linking a senescent immune system to chronic CMV infection and frailty.
|
1) chronic inflammation
2) age-related changes in α-motor neurons,
3) poor nutrition
4) ↓growth hormone (GH) production, sex-steroid levels, and physical activity.
5) Age-related insulin resistance causes an increase of fat infiltration into muscle and a decline in muscle strength.
6) Mitochondrial dysfunction in aging skeletal muscle causes oxidative damage and the decline of energy generation to maintain function properly
|
- Decreased growth hormone and insulin-like growth factor-1 levels in later life (IGF-1)
- Decreased levels of the adrenal androgen dehydroepiandrosterone sulfate (DHEA-S).
- Chronically increased cortisol levels, blunted diurnal variation of cortisol.
- Evidence is mixed that lower levels of the reproductive hormones estrogen and testosterone contribute to frailty.
- there is stronger evidence that links decreased 25(OH) vitamin D levels to f
- railty
|
Management
- Once a frail or prefrail patient is identified there are no succinct guidelines on how to best mange them.
- Diagnosis, differential diagnosis (rule out underlying medical or psychological issues that may be driving signs and symptoms of frailty)
Diagnosing
frailty:
- Laboratory Testing (in order to rule out treatable conditions, A suggested initial screen, based on the differential diagnosis, might include: Complete blood count, basic metabolic panel, liver biochemical tests, including albumin, vitamin B12, vitamin D, and TSH).
Exercise
- Exercise is believed to be the most effective intervention in older adults to improve quality of life and functionality. However, data on specific exercise interventions designed to improve outcomes in patients with frailty are limited.
- The demonstrated benefits of exercise in older adults include increased mobility, enhanced performance of activities of daily living (ADL), improved gait, decreased falls, improved bone mineral density, and increased general well-being.
Nutritional
Supplementation
- In treatment of weight loss, oral nutritional supplements between meals (low-volume, high caloric drinks or puddings) may be helpful in adding protein and calories.
- Vitamin D supplementation for those with low serum vitamin D levels (< 20 ng/ml)is effective for fall prevention, improving balance, and preserving muscle strength.
- those taking leucine-enriched whey protein plus vitamin D had significant improvement in physical frailty related measurements
- Whey protein, omega 3 fatty acids rich items, amino acid glutamine, carnitine have been suggested for their useful role.
Pharmacotherapy
- Not adequately evaluated.
- Such hormonal therapy as testosterone, while it improves muscle strength, has significant systemic side effects. Estrogen-replacement therapy in postmenopausal women also has an unfavorable safety profile.
- Even growth hormone, DHEA, testosterone when deficient, may be considered
- Friedlander et al reported that IGF-1 therapy had a beneficial impact on bone density, muscle strength, or physical function in elderly women with no clinical IGF-1 deficiency.
- Currently available anti-inflammatory agents, while not formally evaluated in clinical trials in treating the frailty syndrome, also have significant adverse effects, particularly in the elderly. Statin has no effect in management of frailty.
- While vitamin D and angiotensin-converting enzyme inhibitors have favorable pharmacological and safety profiles, their clinical utility in the prevention and treatment of frailty has yet to be investigated