Osteoporosis
- Osteoporosis is: ‘progressive loss of bone mass associated with change in bone micro- architecture, leading to enhanced bone fragility and a consequent increase in fracture risk’.
Epidemiology:
- It is estimated that 1 in 3 women and 1 in 12 men over the age of 50 years worldwide suffer from osteoporosis. Above age of 60, one in two women and one in three men will have a minimal trauma fracture because of osteoporosis.
- Associated with excess morbidity and mortality – 33% of people die and 35% require help to walk one year after a hip fracture.
Pathophysiology
- The risk of osteoporosis depends on the peak bone mass attained in young adult life and the rate of bone loss in later years.
- The peak bone mass, excessive bone resorption and inadequate formation of new bone remodeling are the three main mechanisms by which osteoporosis develops.
 Achieving peak bone mass depends on adequate nutrition, appropriate intake of calcium and vitamin D, exercise and regular menstrual cycles.
Achieving peak bone mass depends on adequate nutrition, appropriate intake of calcium and vitamin D, exercise and regular menstrual cycles.
- Remodeling is: A normal process continually taking place within bone to repair micro damage through continuous bone formation and resorption.
 Stages of bone remodeling are:
Stages of bone remodeling are:
1. Activation of osteoclasts from circulating precursor cells, mediated by receptor binding of NF-κB (RANK) ligand.
2. Aggregation and adherence of osteoclasts to regions of active bone resorption on the trabecular plate.
3. Osteoclastic breakdown of bone matrix, releasing calcium, minerals and active growth factors.
4. Simultaneous osteoblastic deposition of osteoid with subsequent mineralization as calcium and phosphate (hydroxyapatite) is deposited.
- In postmenopausal women, there is a shift towards bone resorption, leading to net bone loss. Osteoclasts function in a less regulated manner, perforating through the trabecular plate. There is then no framework for osteoblast activity and structural integrity is lost. This loss of connectivity between the trabecular plates is typical of the microstructural changes associated with osteoporosis.
|
Risk Factors for primary osteoporosis
|
Causes of secondary osteoporosis
|
- female gender
- current smoker
- alcohol intake >3 units/day
- low calcium and vitamin D deficiency
- Low body mass index (<19 kg/m2).
|
Endocrinal: hyperthyroidism/ hyperparathyroidism/ Cushing
rheumatoid arthritis
chronic malabsorption or malnutrition (e.g. coeliac)
Chronic liver disease.
Renal failure
Hematological diseases: multiple myeloma, Leukemia
Drugs: heparin, phenytoin, steroids
|
- In men the major causes of secondary osteoporosis are hypogonadism and corticosteroid therapy.
Possible symptoms:
 Osteoporosis remains asymptomatic till fracture occurs.
Osteoporosis remains asymptomatic till fracture occurs.
 Back pain, caused by a fractured or collapsed vertebra
Back pain, caused by a fractured or collapsed vertebra
 Loss of height over time
Loss of height over time
 A stooped posture (kyphosis)
A stooped posture (kyphosis)
 Fragility fractures
Fragility fractures
- The fracture sites in osteoporosis, the wrist, the hip and the vertebra, have relatively high trabecular bone to cortical bone ratio
Risk stratification tools
- The FRAX tool (http://www.shef.ac.uk/FRAX/) was developed by the World Health Organization as a free-online resource to calculate 10-year fracture risk. These calculations help to inform decisions about treatment alongside investigations.
Investigations
- Blood tests – FBC, UE, LFT, TFT, Ca, PO4, vitamin D, PTH, coeliac serology, myeloma screen.
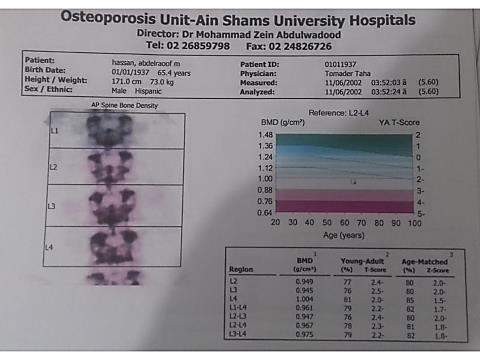
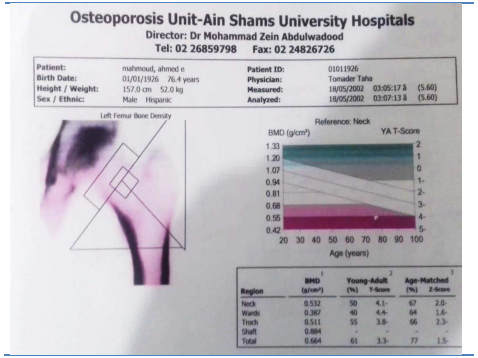
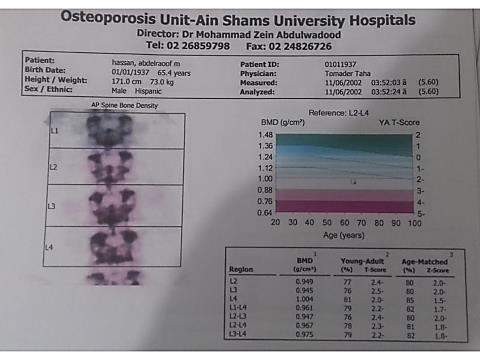
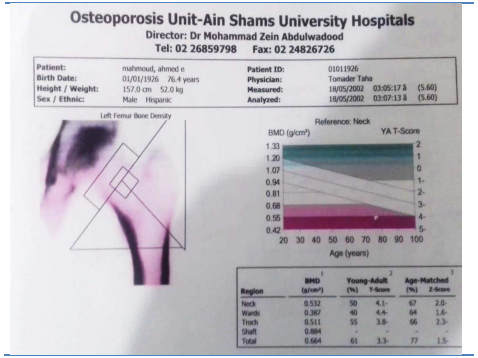
- Dual-energy X-ray absorptiometry (DEXA) scanning is: The gold-standard investigation used to establish a formal diagnosis of osteoporosis by measuring bone mineral density (BMD).
 Reported as a T score, corresponding to the number of standard deviations (SDs) above or below the bone mineral density for an average 25-year-old. A T-score of 2.5 SDs below normal represents osteoporosis.
Reported as a T score, corresponding to the number of standard deviations (SDs) above or below the bone mineral density for an average 25-year-old. A T-score of 2.5 SDs below normal represents osteoporosis.
 Z score, corresponding to the number of SDs above or below the bone mineral density in age-matched controls.
Z score, corresponding to the number of SDs above or below the bone mineral density in age-matched controls.
- A whole-spine X-ray may be helpful to establish the presence of asymptomatic fractures. Up to one-third of vertebral fractures fall into this group.
- Bone turnover markers such as serum C-terminal telopeptide (CTX) levels are used in specialist clinics to establish compliance and effectiveness of treatment.
Management
 Diet rich in calcium and vitamin D
Diet rich in calcium and vitamin D
 Exercise
Exercise
 Stopping smoking
Stopping smoking
 Reducing alcohol
Reducing alcohol
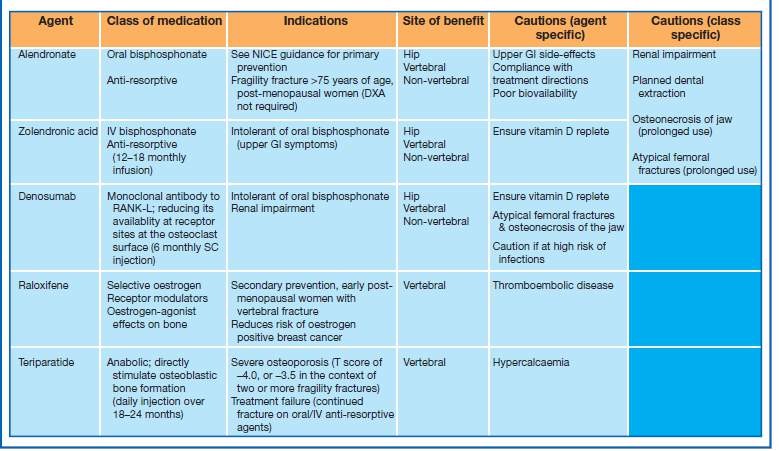
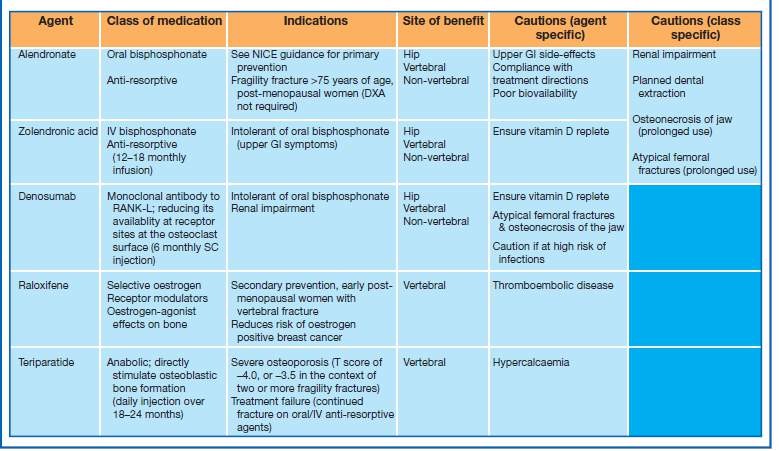
Pharmacological
- All patients with osteoporotic fractures, or at risk of sustaining them, should be commenced on vitamin D supplementation. Co-administration of calcium will depend on baseline serum calcium levels and dietary intake.
- Bisphosphonates are the mainstay of treatment. These inhibit osteoclastic bone resorption. Because the processes are linked, impaired bone resorption results in reduced bone formation and turnover as a whole is reduced. Usually patients receive bisphosphonates for 3–5 years. Beyond this, benefits of therapy must be balanced against risk of atypical subtrochanteric fracture and osteonecrosis of the jaw. Continuation after 3 years depends on a reassessment of fracture risk and up-to-date
- Teriparatide, denosumab and raloxifene are reserved for specific indications
Recommendations for Prescribing Exercise to Patients with Osteoporosis:
Weight-bearing aerobic exercises and muscle-strengthening exercises have been shown to be an integral part of osteoporosis prevention, as well as a part of the treatment process.
All three components of an exercise program are needed for strong bone health: weight-bearing aerobic exercise such as jogging, brisk walking, stair climbing; muscle strengthening exercise with weights; and balance training such as Tai Chi.
Any form of resistance training should be site specific i.e. targeting areas such as the muscle groups around the hip, the quadriceps, dorsi/plantar flexors, rhomboids, wrist extensors and back extensors.
Precautions:
- As many patients may present with comorbidities, it may be necessary to tailor the exercise prescription accordingly.
- There are currently no established guidelines regarding contraindications for exercise for people with osteoporosis. The general recommendation is to prescribe moderate intensity exercise that does not cause or exacerbate pain.
- Exercises that cause twisting (e.g. golf swing), bending or compression of the spine (e.g. rowing or other dynamic abdominal exercises including sit-ups) should also be avoided.
- Exercises that involve high-impact loading should be avoided. Low impact weight-bearing activity is characterized by always having one foot on the floor. Jumping (both feet off floor) is termed high impact training.
QUIZ:
Kindly comment on the following DXA reports