Chronic respiratory diseases (CRDs)
Chronic respiratory diseases (CRDs) are diseases of the airways and other structures of the lung. Some of the most common are asthma, chronic obstructive pulmonary disease (COPD), occupational lung diseases and pulmonary hypertension.
Risk factors:
1. Smoking is the most common risk factor.
2. Genetics: cystic fibrosis, alpha 1 antitrypsin deficiency.
3. Other risk factors include: air pollution, occupational chemicals and dusts, and frequent lower respiratory infections during childhood
4. Connective tissue diseases.
Airway diseases are classified into two groups
|
Obstructive disorders
|
Restrictive disorders
|
|
Characterized by: reduction in airflow.
Shortness of breath in exhaling air.
Air will remain inside the lung after full expiration
|
Characterized by reduction in lung volume
Difficulty in inhaling air
Due to stiffness of lung tissue or limited chest wall expansion
|
|
COPD
Asthma
Bronchiectasis
|
Interstitial lung disease
Marked obesity
Scoliosis
Neuromuscular disorders
|
Clinical presentations can vary with each category:
 Chronic obstructive airway disease: includes both (emphysema and chronic bronchitis): chronic productive cough, dyspnea, fatigue that may progress to respiratory failure and cyanosis. Peripheral oedema, cor pulmonale, respiratory failure and polycythemia may develop in patients with COPD.
Chronic obstructive airway disease: includes both (emphysema and chronic bronchitis): chronic productive cough, dyspnea, fatigue that may progress to respiratory failure and cyanosis. Peripheral oedema, cor pulmonale, respiratory failure and polycythemia may develop in patients with COPD.
 Asthma: condition of airway hyper-responsiveness with reversible airflow obstruction that results in intermittent symptoms of difficult breathing, wheezing, dyspnea, chest tightness, and non- productive cough. Coughing often occurs at night or early in the morning. There are two forms of bronchial asthma (allergic extrinsic and non-allergic intrinsic asthma). Early in the course of the disease, the chest is usually free in between the attacks.
Asthma: condition of airway hyper-responsiveness with reversible airflow obstruction that results in intermittent symptoms of difficult breathing, wheezing, dyspnea, chest tightness, and non- productive cough. Coughing often occurs at night or early in the morning. There are two forms of bronchial asthma (allergic extrinsic and non-allergic intrinsic asthma). Early in the course of the disease, the chest is usually free in between the attacks.
 Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD is a group of respiratory diseases affecting the interstitium of the lungs. It may occur as an abnormal repair process to a variety of injuries to the lungs leading to scarred and thickened alveoli. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. Etiologies could be idiopathic, secondary to connective tissue disease e.g. Sarcoidosis, SLE, Rh A, secondary to lung exposure to inorganic inhalation: silicosis, asbestosis, or organic as Hypersensitivity pneumonitis (Extrinisic allergic alveolitis).
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD is a group of respiratory diseases affecting the interstitium of the lungs. It may occur as an abnormal repair process to a variety of injuries to the lungs leading to scarred and thickened alveoli. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. Etiologies could be idiopathic, secondary to connective tissue disease e.g. Sarcoidosis, SLE, Rh A, secondary to lung exposure to inorganic inhalation: silicosis, asbestosis, or organic as Hypersensitivity pneumonitis (Extrinisic allergic alveolitis).
 Pulmonary hypertension: Is abnormally elevated pressure in the pulmonary circulation. Symptoms of pulmonary hypertension include: shortness of breath, tiredness, feeling faint or dizzy, chest pain (angina), palpitations, edema, and ascites. The symptoms often get worse during exercise. There are five classes.
Pulmonary hypertension: Is abnormally elevated pressure in the pulmonary circulation. Symptoms of pulmonary hypertension include: shortness of breath, tiredness, feeling faint or dizzy, chest pain (angina), palpitations, edema, and ascites. The symptoms often get worse during exercise. There are five classes.
o Class one pulmonary arterial HTN either
1. have no identifiable cause and is then referred to as idiopathic pulmonary hypertension (formerly called primary pulmonary hypertension).
2. Or Drug- and toxin-induced (e.g., methamphetamine use)
3. Or associated with conditions: Connective tissue disease, HIV infection, Portal hypertension, Congenital heart diseases, Schistosomiasis
o Class 2 – Pulmonary hypertension secondary to left heart disease
o Class III – Pulmonary hypertension due to lung disease, chronic hypoxia (COPD, Obstructive sleep apnea, ILD).
o Class IV – chronic arterial obstruction: Chronic thromboembolic pulmonary hypertension.
o class V :Pulmonary hypertension with unclear or multifactorial mechanisms: Sarcoidosis, sickle anemia, glycogen storage disease
 Pulmonary hypertension is diagnosed by measuring the pulmonary pressures by either echocardiogram or right heart catheterization.
Pulmonary hypertension is diagnosed by measuring the pulmonary pressures by either echocardiogram or right heart catheterization.
Investigations to evaluate respiratory system:
Plain chest x-rays are most useful in identifying abnormalities in the heart, lung parenchyma, chest wall, pleurae, diaphragm, mediastinum and hilum. Usually, a chest x-ray is the initial test performed to evaluate the lungs.
Sputum microscopy and serology are useful for the diagnosis of infections of the lungs.
Flow rate and lung volume measurements are used to differentiate obstructive from restrictive pulmonary disorders, to characterize disease severity and to measure responses to therapy. Obstructive lung disorder is characterized by a decrease in the flow rate, whereas restrictive lung disorder is a reduction in lung volume.
Arterial blood gas exchange analysis is useful in assessing accurate measures of PaO2, PaCO2 and blood pH.
A Ventilation and perfusion scan, also called a v/q lung scan, is a type of medical imaging using scintigraphy and medical isotopes to evaluate the circulation of air and blood within a patient's lungs in order to determine the ventilation/perfusion ratio. The ventilation part of the test looks at the ability of air to reach all parts of the lungs, while the perfusion part evaluates how well blood circulates within the lungs.
CT scan: CT scans of the chest define intrathoracic structures and abnormalities more clearly than do chest x-rays. CT angiography using a bolus of intravenous contrast is employed to highlight pulmonary arteries, useful in the diagnosis of pulmonary embolism.
Treatment:
Treatments for each chronic respiratory disease vary and the ideal solution is the reduction and avoidance of risk factors. Neither asthma nor chronic obstructive pulmonary disease (COPD) can be cured but treatments can reduce symptoms, prevent escalation and improve quality of life.
- Smoking cessation
- Supplemental oxygen should be prescribed for patients with PaO2 of 55 mmHg or less. Oxygen should also be used in patients whose O2 saturation drops below 90% during exercise or sleep.
- Asthma: based on avoidance of triggers, Bronchodilators (salbutamol inhalers and steroid inhalers, such as beclometasone) using spacers or dry powder preparations, long acting β-agonist (salmeterol) inhalers, and theophylline are effective.
- COPD: use of bronchodilators, antibiotics, inhaled corticosteroids, mucolytics.
- ILD is multiple conditions, hence treatment is different for each disease. If a specific occupational exposure cause is found, the person should avoid that environment. If a drug cause is suspected, that drug should be discontinued. Many cases due to unknown or connective tissue-based causes are treated with corticosteroids, such as prednisolone. Some people respond to immunosuppressant treatment.
- Pulmonary hypertension: treat the cause, diuretics, anticoagulation, vasodilators (prostacyclin, sildenafil, calcium channels blockers), Endothelium antagonists are the newest medications used for this condition. These include bosentan and ambrisentan.
Role of physiotherapy:
1. Proper assessment and exclude acute on top of chronic conditions as infection, acute exacerbation of COPD or acute asthma attack.
2. Screen for other comorbidities e.g. hypertension, IHD, or DM.
3. Stop smoking.
4. Nutritional counseling.
5. Vaccination pneumococcal, influenza.
6. Control environmental exposure to air pollution.
7. warm up and use of bronchodilators to avoid exercise- induced bronchospasm in asthma
8. Diaphragmatic breathing (to retrain the patient to use the diaphragm more than the chest muscles).
9. Positioning changes can be used to address ventilation and perfusion mismatches and to help with postural drainage.
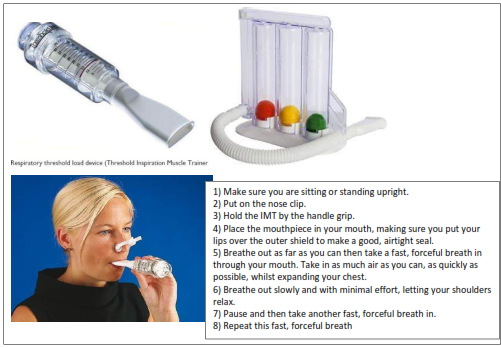
10. Inspiratory muscle training is specifically directed at inspiratory muscles. It is usually performed by breathing in against a measured resistance using a specific device. It is uncertain how much, or if, inspiratory muscle training adds to a whole- body exercise programme, but it is known to be effective alone and is potentially useful for individuals who are unable to cycle or walk.
11. More efficient coughing techniques can be taught to help expel secretions. This will help prevent pooling of secretions, subsequent infections, or air trapping. Manual chest therapy, including percussion or a vibrator, can help mobilize secretions.
12. A pulmonary rehabilitation program should include endurance and/or reconditioning exercises. For these the therapist needs to monitor the patient’s heart rate and oxygen saturation. The heart rate should be limited, generally as a percentage of an age-adjusted maximal heart rate (this is especially important for patients with additional cardiac disease).
13. Oxygen saturation should be monitored as well as the patient’s perceived exertion. Exercise should be discontinued for O2 saturation below 90%, significant increases in exertion or dyspnea, chest pain, or tachycardia or irregular heart rate.
14. Therapy should be performed 3–5 days per week. Walking is a fundamental part of a pulmonary rehabilitation, and patients should be encouraged to walk outside of therapy (with appropriate precautions and oxygen supplementation if required).
15. An exercise bicycle may also be beneficial for home use. An important part of therapy is for patients to learn their abilities and limitations so they can safely exercise at home. Physical or occupational therapists should also help develop an upper body exercise program.
16. Occupational therapists may be helpful in assessing activity of daily living (ADL) impairments and with prescribing assistive devices. Respiratory therapists can help instruct patients in the proper use of medications and mobilization of secretions and teach them breathing techniques. In pulmonary patients, nutritional evaluations may also be needed.