Cardiovascular conditions
1. Systemic Hypertension
- Hypertension is diagnosed when a person’s systolic blood pressure (SBP) in the office is ≥140 mm Hg and/or their diastolic blood pressure (DBP) is ≥90 mm Hg following repeated examination.
- The measurement of BP should be done at least twice on at least two subsequent visits under complete mental & physical rest.
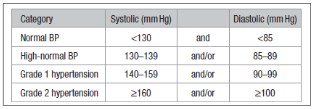
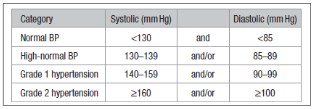
Staging of Blood pressure
Symptoms
- There is usually none. An elevated BP is most frequently just found on a routine examination.
1. Headache: frontal or occipital headaches are typically worse in the morning
2. Dizziness or light-headedness
3. Dyspnoea on effort
4. Angina (increased muscle mass + coronary disease)
5. Mild visual disturbance
6. Epistaxes.
Types and causes of systemic hypertension:
- Systolic & diastolic hypertension.
- Essential (95% of cases): family history +ve
- Secondary hypertension: where blood pressure elevation is the result of a specific cause:
- Renal artery stenosis, glomerulonephritis, pyelonephritis, polycystic disease.
- Phaeochromocytoma, Primary hyperaldosteronism (Conn syndrome), Cushing syndrome, Acromegaly, Hypercalcaemia.
- Coarctation of the aorta, Polyarteritis nodosa
- Pre-eclampsia
- Iatrogenic drug therapy: glucocorticoids, MAOIs, sympathomimetics, oestrogens
Complications
- Hypertension is associated with an increased risk of cerebrovascular disease, retinopathy, cardiac failure, MI, occlusive peripheral arterial disease, and renal failure. Each increment of 10 mmHg systolic pressure reduces life expectancy.
Investigations
- Almost all patients will have essential hypertension (? family history) and the necessary investigations are: CBC, urea, creatinine, electrolytes, Urine testing: protein, blood, sugar; ECG.
- Investigate other cardiovascular risks (diabetes, hyperlipidemia)
- Investigate for complications (Fundus examination, Echocardiography,….).
Management
Non pharmacological lines of treatment:
- Weight reduction for obese patients.
- Stop smoking, moderate coffee and alcohol intake.
- Salt restriction in diet.
- Regular exercise.
- Avoid stress, Relaxation and biofeedback.
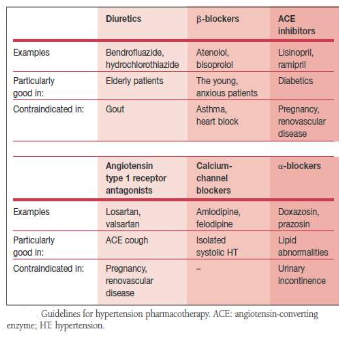
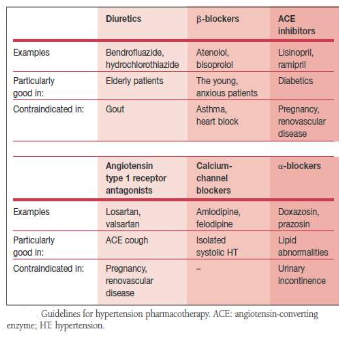
Pharmacological lines of treatment: See Figure Treatment of the cause in secondary hypertension Treatment of complications
Exercise program:
- For aerobic exercise, 5-7 d/wk, supplemented by resistance exercise 2-3 d/wk and flexibility exercise ≥2-3 d/wk.
- For aerobic exercise, a minimum of 30 min or up to 60 min/d for continuous or accumulated aerobic exercise. If intermittent, begin with a minimum of 10 min bouts.
- Aerobic exercise should be at least at moderate intensity (e.g. brisk walking), corresponding approximately to 40 to 60% of maximal aerobic capacity (VO2max). Resistance exercise should be at moderate intensity, which could be expressed as 50 to 70% of 1-repetition maximum.
Blood pressure response to exercise session:
- During exercise your muscles demand more oxygen. To meet this need, the heart must pump with increased force to deliver more oxygenated blood with each contraction. As the heart’s workload increases during exercise, systolic blood pressure increases.
- Systolic blood pressure measures the force against artery walls when the heart pumps. It is normal for systolic blood pressure to range between 160 and 220 during exercise.
- The diastolic blood pressure typically does not change during exercise. Diastolic pressure measures the force against artery walls in between contractions. If diastolic blood pressure increases during exercise by more than 20 mm Hg or becomes greater than 100 mm Hg, stop exercising and consult physician.
- A cool down period post exercise to avoid sharp drops in blood pressure. A cool down period gradually brings heart rate and blood pressure back to normal.
It is normal for blood pressure during exercise to increase. It should return to normal post exercise.
Precautions:
1. Monitor for blood pressure control to target levels. If arterial hypertension is poorly controlled (resting systolic BP>160 mmHg), high-intensity exercise training as well as maximal exercise testing should be discouraged or postponed until appropriate drug treatment has been instituted and arterial BP is lowered.
2. Monitor for drug side effects:
1. vasodilators can cause orthostatic hypotension
2. β-blockers and diuretics may adversely affect thermoregulatory function and cause hypoglycaemia in some individuals. In these situations, educate patients about the sign and symptoms of heat intolerance and hypoglycaemia, and the precautions that should be taken to avoid these situations.
3. Antihypertensive medications such as calcium channel blockers, β-blockers and vasodilators may lead to sudden reductions in post-exercise blood pressure. Extend and monitor the cool-down period carefully in these situations.
4. β-blockers, particularly the non-selective types, may reduce sub-maximal and maximal exercise capacity primarily in patients without myocardial ischaemia. Consider using perceived exertion to monitor exercise intensity in these individuals.
3. Gradual progression
- To avoid injury, progression of frequency and intensity of resistance exercise should occur slowly. Gradual progression of intensity of aerobic exercise is also advisable to enhance compliance.
4. Intensive isometric exercise such as heavy weight lifting can have a marked pressor effect and should be avoided. Avoidance of the Valsalva maneuver in particular is warranted. This maneuver is characterized by significant increments in intrathoracic pressures leading to (greater) elevations in (especially) systolic and diastolic blood pressure, when holding the breath during muscular contraction.
5. Hypertensive patients are at increased risks of myocardial ischemia. Hypertensive patients should be informed about the nature of cardiac prodromal symptoms and exercise-related warning symptoms including chest pain or discomfort, abnormal dyspnoea, dizziness or malaise, and should seek prompt medical care if such symptoms develop.