2. Orthostatic Hypotension
Orthostatic hypotension (OH) is defined as a drop in systolic blood pressure by 20 mmHg or diastolic blood pressure by 10 mmHg, compared to supine blood pressure, within 3 min of standing.
The prevalence of OH is reported to be between 5% and 30%.
Clinical implications:
1. OH is a risk factor for syncope, falls, cognitive impairment and hospitalization.
2. OH is also an independent predictor of mortality in older persons.
3. OH is an important consideration in the treatment of hypertension in older persons, as cardiovascular drugs are a common cause of OH.
Normal response to orthostatic stress:
Changing from supine to erect position results in venous pooling of blood. With the change in position, the baroreceptors precipitate an increase in medullary sympathetic outflow resulting in vasoconstriction of the systemic resistance vessels and splanchnic vessels, a compensation for the orthostatic stress.
Age related changes predispose to orthostatic hypotension:
- Decreased autoregulation of cerebral blood flow.
- Blunted baroreceptor response.
- Decreased heart rate response to orthostatic stress due to decreased beta receptors.
- Decrease in basal and stimulated renin levels and aldosterone production with increases in atrial natriuretic peptide in the elderly lead to increased risk of volume and sodium depletion.
Causes:
OH in older persons is often multifactorial; contributing causes include:
- volume depletion: dehydration (vomiting- diarrhea- 3rd space loss- hemorrhage)
- anemia,
- prolonged bed rest
- autonomic neuropathy (e.g., diabetes, amyloidosis, alcohol, uremia, vitamin B deficiency),
- Primary autonomic failure, Parkinson’s disease, stroke,
- cardiac disease (MI- heart failure)
- Endocrinopathies such as hypoadrenalism
- Medications: diuretics causing volume depletion, alpha blockers used for prostatic enlargement,
Presentations:
Since older adults are usually asymptomatic (e.g., they don’t complain of lightheadedness) and orthostatic pressures are usually not routinely measured unless there is clinical suspicion, it is frequently missed. Patients may present with light-headedness, blurred vision, dizziness, weakness, and fatigue, or with syncope. Less commonly, they may present with neck and shoulder pain, orthostatic dyspnea, and chest pain. It can be associated with postprandial hypotension.
Management:
1. Evaluation should begin by identifying reversible causes and underlying associated medical conditions.
2. Blood pressure should be measured supine and 3 min after standing.
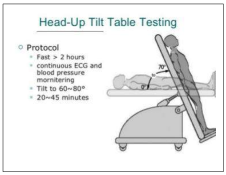
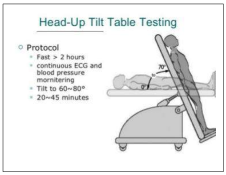
3. Head-up tilt table testing should be considered where there is a high pretest probability of OH despite negative bedside evaluation and in patients who are unable to stand for blood pressure measurement
4. Non-pharmacologic management includes discontinuing potential medications contributing to OH, ensuring adequate hydration and sodium, coffee intake (be careful in systemic hypertension).
5. Avoid prolonged standing, hot environment and showers, and alcohol intake.
6. Teaching physical maneuvers (e.g., squatting, bending at waist), and abdominal and lower limb binders. Elevating the head of the bed up to 20.3 cm (8 in) for sleeping and using elastic garments.
7. Exercise program to improve conditioning, swimming might be an ideal exercise, as the hydrostatic pressure of the water counteracts the hypotension the patient is experiencing.
a. During a PT session, it will be important to monitor a patient's BP before, during, and after exercise. It will also be necessary to choose appropriate exercises and environment to avoid these symptoms from occurring.
b. Teaching gradual standing technique. Exercise the calf muscles before sitting up, and sit on the edge of the bed for a few minutes before standing to give the body time to adjust to the postural change and help the blood flow back to the heart.
c. Advise the patient to refrain from quick postural changes, scheduling activities for later in the day.
d. Avoid bending at the waist to pick up items from the floor or to reach for something on a lower shelf. If possible, squat at the knees and keep the head above the level of the heart.
8. Patients with postprandial symptoms should be advised to avoid large carbohydrate meals
9. In patients with persistent symptoms despite these measures, a trial of pharmacologic therapy is indicated. Fludrocortisone is often used as the first line. Other treatment options include midodrine and other alpha-adrenergic agents, desmopressin, octreotide, and erythropoietin.