Congestive Heart Failure (CHF)
A complex syndrome caused by a structural or functional abnormality in the cardiac muscle that impairs its ability to function as a pump and meet the metabolic needs of the body.
Etiology of CHF
|
Systolic Dysfunction (inability to expel blood)
|
Diastolic Dysfunction (abnormal filling)
|
|
Hypertension
|
Hypertension
|
|
Ischemic heart disease
|
Fibrosis
|
|
Cardiomyopathy
|
Ischemia
|
|
Valvular disease
|
Aging process
|
|
Myocarditis
|
Constrictive pericarditis (like TB)
|
|
|
Hypertrophic cardiomyopathy
|
Types of heart failure
Left-sided heart failure: This causes a reduction in LV output and/or an increase in the left atrial or pulmonary venous pressure.
An acute increase in left atrial pressure may cause pulmonary oedema; a more gradual increase leads to reflex pulmonary vasoconstriction and pulmonary hypertension.
Right-sided heart failure (e.g. chronic lung disease, multiple pulmonary emboli): This causes a reduction in right ventricular (RV) output for any given right atrial pressure.
Biventricular heart failure: This may develop because disease affects both ventricles (e.g. dilated cardiomyopathy), or because left heart failure leads to chronic elevation of left atrial pressure, pulmonary hypertension and right heart failure. Heart failure may develop suddenly (acute heart failure) or gradually (chronic heart failure).
High output failure: This may occur with large arteriovenous shunts or thyrotoxicosis, due to an excessively high cardiac output.
‘Compensated heart failure’: This term describes a patient with impaired cardiac function in whom adaptive changes have prevented the development of overt heart failure.
Clinical picture:
1. Symptoms and signs due to systemic venous congestion(edema, congested neck vein, congested hepatomegaly, dyspepsia, ascites)
2. Symptoms and signs due to pulmonary venous congestion(dyspnea on exertion progress to dyspnea at rest, orthopnea, Paroxysmal nocturnal dyspnea, cough, expectoration, pulmonary edema)
3. Symptoms and signs due to low cardiac output )fatigue, dizziness and a poor effort tolerance; the peripheries are cold and BP is low)
4. In advanced heart failure a number of non-specific complications may occur:
a. Marked weight loss (cardiac cachexia) is caused by a combination of anorexia and impaired absorption due to GI congestion.
b. Renal failure arises from poor renal perfusion due to a low cardiac output and may be exacerbated by diuretic therapy, ACE inhibitors and angiotensin receptor blockers.
c. Atrial and ventricular arrhythmias are very common and may be related to electrolyte changes (e.g. hypokalaemia, hypomagnesaemia), underlying structural heart disease, and the pro-arrhythmic effects of sympathetic activation. Sudden death occurs in up to 50% of patients, often due to ventricular arrhythmias.
Causes of CHF exacerbation/decompensation: FAILURE
F: forgot to take medication, ran out of medication
A: arrhythmias (especially atrial fibrillation)
I: ischemia / infarction / infection
L: lifestyle (poor diet)
U: up-regulation (high cardiac output states i.e. pregnancy, thyrotoxicosis, anemia)
R: renal failure (fluid overload)
E: embolism / endocarditis Diagnosis
- History and clinical examination
- Echocardiography -wall thickness, cavity dimensions, ventricular function ( systolic and diastolic), can reveal underlying etiology
- ECG-Commonly abnormal, Q waves, ST/T changes, LVH, arrhythmias and axis change
- Brain natriuretic peptide (BNP): elevated in heart failure and can be used as a screening test in breathless patients and those with edema
Treatment
1. Dietary instruction: Sodium restriction and limited fluid intake.
2. Diuretics
3. Beta-blockers reduces mortality
4. Positive inotropic agents: digoxin improves symptoms, does not reduce mortality
5. Angiotensin-converting enzyme: vasodilator decreased preload and afterload
6. Aldosterone antagonists
Exercise Guidelines for CHF
- The key point here is to provide a moderate intensity of exercise to gain positive results. Many times, clinicians are nervous to push the patients to their moderate intensity level due to fatigue or exhaustion.
- Maximum heart rate should be between 60 % to 80% in order to achieve favorable results with CHF (careful for beta blockers).
- Low-level exercises can start when the patient’s functional status of the cardiac system (hemodynamic system) is stable. Exercises should consider the patient’s systemic conditioning, peripheral endurance training, low-level resistance training, and respiratory muscle training.
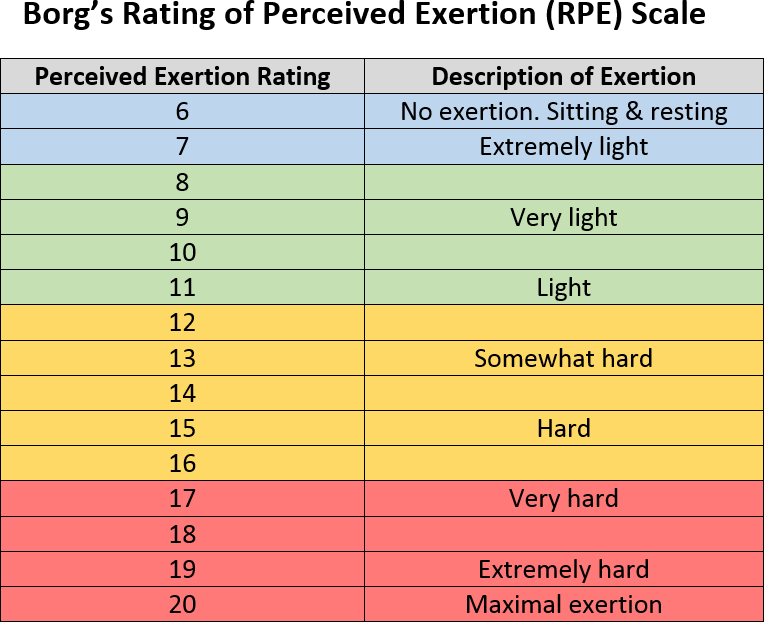
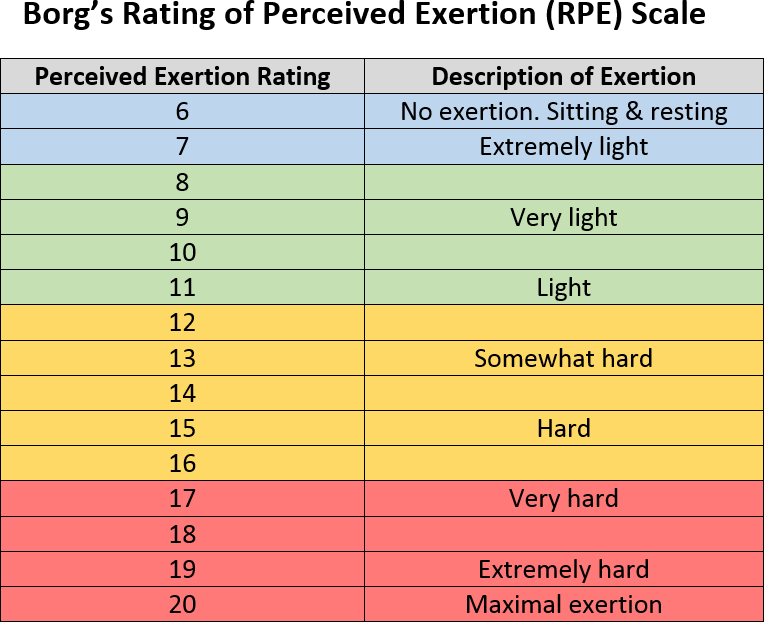
- During exercises, the patient needs to be monitored through oxygen saturation (using pulse oximetry with finger probe), vital signs (BP, HR, RR), observation, auscultation, and recording the RPE (Borg RPE scale). Also, the patient needs to be observed for orthostatic hypotension caused by exertion and significant dysrhythmias.
- The exercise intensity should start low; the duration of exercise can be gradually increased as per the patient’s tolerance. The exercise HR should be less than 115 bpm. Considering the patient’s medications (and that the exercises do not increase the HR more than 10–20 bpm), the best method for monitoring patient’s exercise intensity is the RPE scale.
- For patients who are deconditioned, light calisthenics in sitting position are recommended to begin the exercise program. (Pull-ups, Chin-ups, Jump squats, Pushups). Also, the exercises need to start with a prolonged warm-up and end with a prolonged cool-down. Isometrics are contraindicated.
- Resistance training can start with elastic bands (yellow) or light weights for the upper and lower extremities.
Discontinue Cardiac Interventions if :
- Temperature of more than 37.7o C
- Systolic BP of more than 240 mm Hg
- Diastolic BP of more than 110 mm Hg
- Fall in systolic BP of more than 20 mm Hg
- Rise in HR of more than 20 bpm
- Resting HR of more than 130 bpm and/or less than 40 bpm
- Chest pain, palpitations, and/or irregular pulse
- Oxygen saturation of less than 90%
- Blood glucose of more than 250 mg/dL
- Cyanotic and/or diaphoretic
- Dizziness and/or syncope
- Bilateral leg/foot edema