Metabolic Syndrome
Metabolic Syndrome (MetS) is defined by a constellation of an interconnected physiological, biochemical, clinical, and metabolic factors that directly increases the risk of atherosclerotic cardiovascular disease (ASCVD), T2DM, and all-cause mortality.
According to the National Cholesterol Education Program Adult Treatment Panel (NCEP/ATP), MetS is a condition that is diagnosed when a patient has any three of the following: elevated fasting glucose ≥110 mg/dL, high TGs ≥ 150 mg/dL, low HDL (<40 mg/dL for men, <50 mg/dL for women), hypertension > 130/85 mm Hg, and abdominal obesity (waist circumference > 88 cm in men, >102 cm in women).
Epidemiology:
The prevalence of MetS (based on NCEP-ATP III criteria, 2001) varied from 8% to 43% in men and from 7% to 56% in women around the world.
MetS confers a 5-fold increase in the risk of type 2 diabetes mellitus (T2DM) and 2-fold the risk of developing cardiovascular disease (CVD) over the next 5 to 10 years. Further, patients with the MetS are at 2- to 4-fold increased risk of stroke, a 3- to 4-fold increased risk of myocardial infarction (MI), and 2- fold the risk of dying from such an event compared with those without the syndrome. The risk increases with the number of MetS components present.
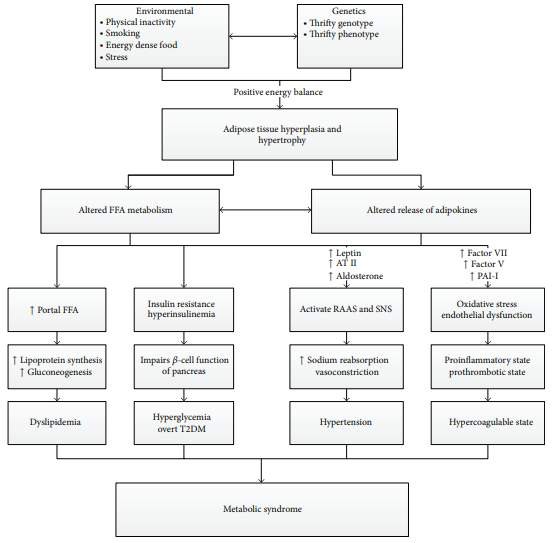
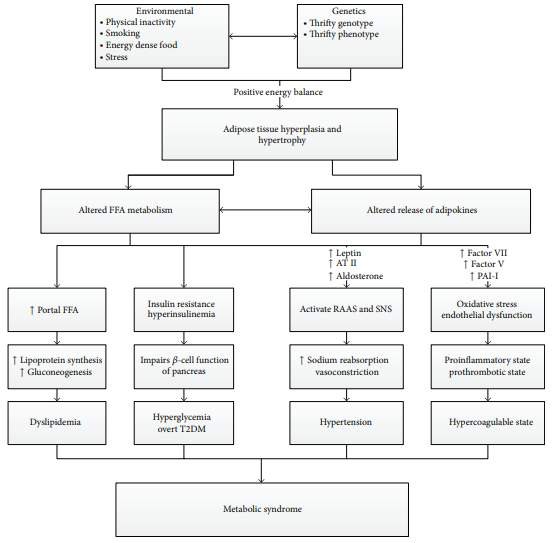
Pathophysiology of MetS (see figure)
MetS is a state of chronic low grade inflammation as a consequence of complex interplay between genetic and environmental factors.
1. Insulin resistance.
2. Visceral adiposity
3. Atherogenic dyslipidemia
4. Endothelial dysfunction
5. Genetic susceptibility
6. Elevated blood pressure
7. Hypercoagulable state
8. Chronic stress
Systemic effects of MetS
|
Renal
|
Microalbuminuria, hypofiltration, hyperfiltration, glomerulomegaly, focal segmental glomerulosclerosis, and chronic kidney disease
|
|
Hepatic
|
Increased serum transaminase, nonalcoholic steatohepatitis (NASH), nonalcoholic fatty liver disease (NAFLD), hepatic fibrosis, and cirrhosis
|
|
Skin
|
Acanthosis nigricans, androgenetic alopecia, skin tags, skin cancer
|
|
Ocular
|
Nondiabetic retinopathy, age related cataract, central retinal artery occlusion, primary open angle glaucoma, oculomotor nerve palsy, and lower lid entropion
|
|
Sleep
|
Obstructive sleep apnea
|
|
Cardiovascular system
|
Coronary heart disease (CHD), myocardial infarction (MI), and stroke
|
|
Reproductive system
|
Hypogonadism, polycystic ovarian syndrome (PCOS), and erectile dysfunction
|
|
Cancers
|
Breast, pancreas, and prostrate
|
|
Gout
|
Raised uric acid levels (Hyperuricemia)
|
Pathophysiology of MetS
The pathogenesis of the atherosclerotic plaque and arterial thrombosis:
LDL can be modified by oxidation. Scavenger macrophages located beneath the intimal surface of arteries engulf oxidized LDL, becoming lipid-laden foam cells, which secrete growth factors that stimulate smooth muscle cell proliferation. These developing plaques also secrete cytokines that attract inflammatory cells, which secrete proteolytic enzymes; these enzymes erode the fibromuscular plaque cap, making it prone to rupture.
When rupture occurs, platelets aggregate and release chemicals that promote vasoconstriction and initiate thrombus formation, which may ultimately occlude the artery.
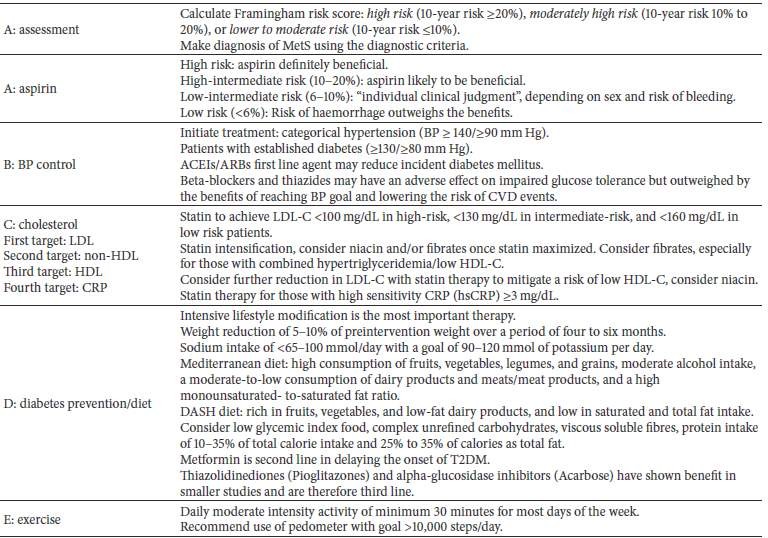
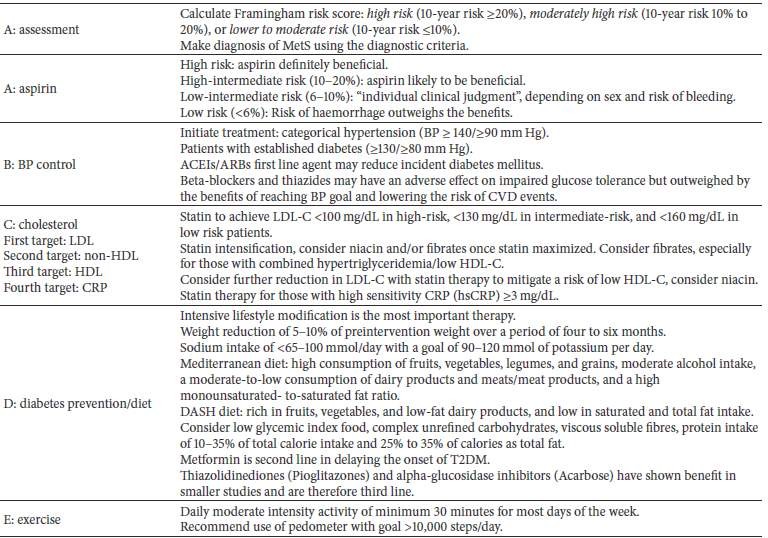
Multidisciplinary approach to the MetS