Diabetes Mellitus
Diabetes mellitus (DM) refers to a group of metabolic disorders characterized by chronic hyperglycemia and disturbances of carbohydrate, protein, and fat metabolism that result from inadequate production and/or impaired action of insulin.
Etiology and classification:
Primary:
- Type 1: previously called Insulin-dependant DM (IDDM) or juvenile-onset DM (In genetically susceptible individuals: HLA-DR3 and/or -DR4, one or more environmental factors viruses e.g. coxsackie, rubella, mumps trigger immune-mediated destruction of islet β cells (insulinitis) leading to complete deficiency of insulin. Autoantibodies are present: ICA:Islet cell antibodies are present in around 90% of newly diagnosed type 1 diabetics. Other antibodies present include GAD: Glutamic acid decarboxylase, tyrosine phosphate antibodies and IAA: insulin autoantibodies).
- Type 2: previously called non insulin-dependant DM (NIDDM) or adult-onset DM: the principal abnormality is insulin resistance, Strongly linked with the rising prevalence of obesity.
- MODY : mature onset diabetes in young patient Secondary:
- Pancreatic causes e.g. Chronic pancreatitis, cystic fibrosis, hemochromatosis.
- Endocrinal: Cushing , Acromegaly , Thyrotoxicosis.
- Drugs : Cortisone, Thiazide
- Others : Gestational diabetes
Presentations:
 The most common presentation of diabetes is related to hyperglycemia and the effects of urinary loss of glucose. Patients present with polyuria, polydipsia, or polyphagia, weight loss.
The most common presentation of diabetes is related to hyperglycemia and the effects of urinary loss of glucose. Patients present with polyuria, polydipsia, or polyphagia, weight loss.
 Type 2 diabetics are far more likely to be asymptomatic at presentation.
Type 2 diabetics are far more likely to be asymptomatic at presentation.
 Both types are associated with vulvovaginal candidiasis, blurry vision, peripheral neuropathy, erectile dysfunction, and generalized fatigue and weakness.
Both types are associated with vulvovaginal candidiasis, blurry vision, peripheral neuropathy, erectile dysfunction, and generalized fatigue and weakness.
 Unfortunately, some patients still present as medical emergencies with acute decompensation of their previously unrecognized diabetic state e.g. diabetic ketoacidosis, hyperosmolar non-ketotic coma. It is important to examine for evidence of a precipitating cause, e.g. infection or myocardial infarction.
Unfortunately, some patients still present as medical emergencies with acute decompensation of their previously unrecognized diabetic state e.g. diabetic ketoacidosis, hyperosmolar non-ketotic coma. It is important to examine for evidence of a precipitating cause, e.g. infection or myocardial infarction.
Screening for Diabetes Mellitus
Asymptomatic adults should be screened for DM if they have a BP greater than 135/80, obesity, proteinuria, previous Gestational DM, or family history.
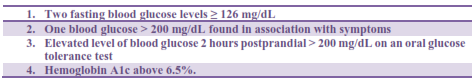
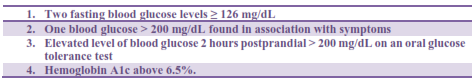
Diagnostic tests: The screening methods and the criteria for the diagnosis are the same:
Complications:
1. Acute metabolic complications:
a) Hypoglycemia
b) Hyperglycemia: diabetic ketoacidosis, hyperosmolar non-ketotic coma
2. Chronic complications:
- Macrovascular complications: cerebrovascular disease, coronary heart disease, and peripheral heart disease.
- Microvascular complications: peripheral neuropathy, autonomic neuropathy, proliferative retinopathy, nephropathy.
Autonomic neuropathy manifests as erectile dysfunction, gastroparesis, constipation/ diarrhea, incontinence, orthostatic hypotension, and/ or sweating abnormality.
Diabetic foot due to ischemia, loss of sensation, infection on top of minor trauma.
COMMONLY ASSOCIATED CONDITIONS
Hypertension, hyperlipidemia, metabolic syndrome, fatty liver disease, infertility, Polycystic ovary syndrome, acanthosis nigricans.
Management:
1. Calorie reduction with physical activity sufficient to produce a 7% to 10% weight loss.
2. Smoking cessation
3. Aspirin: treatment for secondary prevention of IHD
4. If 40 to 75 years old, begin a statin
5. Targets of metabolic control:
a. Low-density lipoprotein cholesterol levels less than 100 mg/dL or less than 70 mg/dL in very high- risk patients.
b. High-density lipoprotein cholesterol levels for men higher than 40 mg/dL and women higher than 50 mg/dL.
c. Triglyceride levels lower than 150 mg/dL.
d. Hemoglobin A1c < 7% as close to normal as possible without causing significant hypoglycemia.
e. Blood pressure <130/80 mm Hg: ACE inhibitor/ARB first-line antihypertensives to prevent albuminuria and nephropathy.
6. Diabetes self-management education: self-monitoring, prevention of complications.
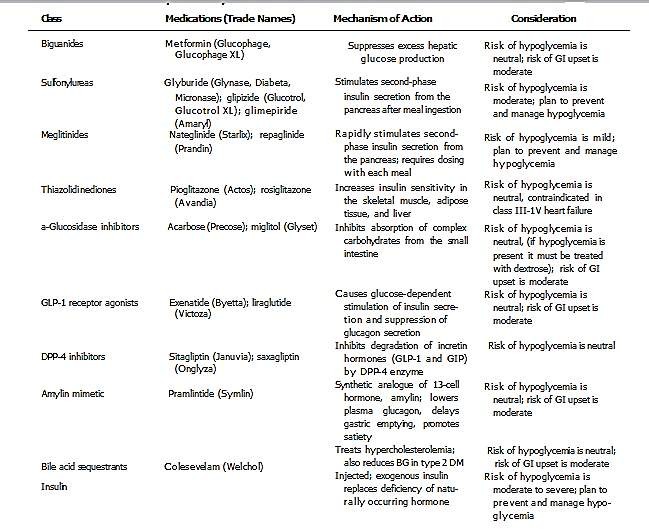
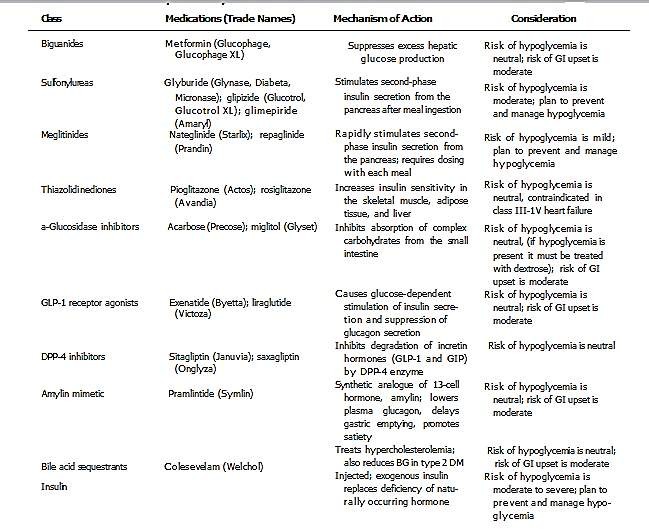
7. Pharmacological therapy: antidiabetic medications and insulin (see tables)
|
Insulin Preparation
|
Onset of Action
|
Peak
|
Duration of Action
|
|
Aspart (NovoLog); lispro (Humalog); glulisine (Apidra)
|
About 5-15 min
|
1-2 h
|
4-6 h
|
|
Human regular insulin (Humulin R, Novolin R)
|
30-60 min
|
2-4 h
|
6-8 h
|
|
Human NPH ( Humulin N, Novolin N)
|
2-4 h
|
4-10 h
|
12-20 h
|
|
Detemir (Levemir)
|
1-2 h
|
Relatively flat
|
Up to 24 h
|
|
Glargine (Lantus)
|
1-2 h
|
Flat
|
Up to 24 h
|
|
Mixed insulins
|
|
|
|
|
Novolin 70/30
|
30-60 min
|
Varies
|
10-16 h
|
|
Humulin 70/30
|
30-60 min
|
Varies
|
10-16 h
|
|
Novolog 70/30
|
5-15 min
|
Varies
|
10-16 h
|
|
Humalog 75/25
|
10-15 min
|
Varies
|
10-16 h
|
Physical therapy needs for Diabetic patients
- Increased incidence of tendonitis
- Increased incidence of frozen shoulder
- Obesity
- Peripheral neuropathy
- Muscle weakness
- Imbalance and increased risk for falls
- Cardiovascular risk
- Depression and stress
Precautions for physical therapy in Diabetic patients:
1. Exercise may cause hypoglycemia be careful with those have previous asymptomatic hypoglycemia. Snacks high in carbs, juice, or sugar cubes should be available for patients in care of blood sugar lows during PT.
2. Exercise may interfere with timed insulin uptake if performed in area of injection site soon after injecting.
3. PT should inquire if medication is taken, when, and where (if insulin is injected) to avoid facilitating rapid uptake if patient has eaten appropriately; if patient has glucose testing monitor with them for monitoring
- If glucose > 300, exercise should be avoided
- If glucose 250 to 300, exercise should be performed with caution
4. Orthostatic hypotension is common due to autonomic neuropathy. should avoid dehydration during exercise by drinking 0.4–0.8 L water during the exercise bout.
5. Diabetes is a major risk factor for cardiovascular disease; people with diabetes are 2 to 4 times more likely to have cardiovascular disease than people without DM. People with diabetes, particularly of long duration, are susceptible to autonomic neuropathy and are less likely to have symptoms, for example, angina while experiencing myocardial ischemia; therefore, exercise training tailored by the recognition of symptoms of myocardial ischemia is not straightforward in these patients; indeed, some patients can have a large area of ischemic myocardium before having any chest discomfort or angina equivalent
6. Some people with diabetes may have developed long-term complications that make cardiopulmonary rehabilitation more challenging; examples include:
a) Blindness
b) peripheral neuropathy with decreased sensation
c) peripheral vascular disease with significant claudication or digit/limb amputation
d) cardiac autonomic neuropathy, characterized by resting tachycardia, inability to increase the heart rate in response to exercise
e) Orthostatic (postural) hypotension.
7. Ergonomic casts or splints for neuropathic hand or feet